0346
Deformation-field magnetic resonance imaging for non-invasive evaluation of disc deformation in vivo1Institute of Clinical Sciences, University of Gothenburg, Gothenburg, Sweden, 2Medical Physics and Biomedical Engineering, Sahlgrenska University Hospital, Gothenburg, Sweden, 3Department of Radiology, Sahlgrenska University Hospital, Gothenburg, Sweden, 4Department of Orthopaedics, Sahlgrenska University Hospital, Gothenburg, Sweden
Synopsis
In vivo evaluation of the intervertebral disc (IVD) during spinal loading may yield greater insight into the biomechanical properties of the IVD. This study aimed to investigate how the lumbar IVD deforms during loading, quantified with a novel non-invasive method utilizing MRI and image registration. Findings showed that the intradiscal deformation depends not only on disc degeneration but also on the lumbar spine level. This highlights the need for tools that can evaluate the mechanical properties of the disc in vivo. The proposed method offers a possibility to depict and track biomechanical changes non-invasively while characterizing disc structures in detail.
Introduction
The response of the intervertebral disc (IVD) to mechanical stimuli in vivo remains largely undocumented. Ex vivo experiments are not adequate surrogates for in vivo studies as they cannot capture the IVD’s biomechanics at native loading conditions. Methods for evaluation of the biomechanical properties of the IVD in vivo may yield greater insight into the pathophysiology of the IVD and possibly improve spinal diagnostics. Magnetic resonance imaging (MRI) provides a non-ionizing and non-invasive tool for in vivo evaluation and when performed during axial loading of the spine it may reveal important intradiscal deformation patterns. The purpose was to investigate how the lumbar IVD structure deforms in vivo during spinal loading, quantified with a novel non-invasive method utilizing MRI and image registration.Methods
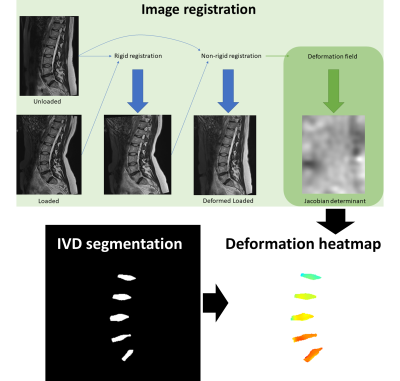
MR images of the lumbar spine (L1-S1), of 24 patients suffering from chronic low back pain (LBP) and 12 controls, were acquired with a 1.5 T scanner. T2-weighted images were acquired at unloaded and loaded state using a compression device (DynaWell Diagnostics Inc) to evaluate the IVD properties at different spinal levels, with diverse degeneration. The degree of IVD degeneration was evaluated according to the Pfirrmann scheme [1].The lumbar spine images acquired during axial loading were rigidly and non-rigidly transformed to corresponding unloaded T2-weighted MR images using Elastix (Vers.5.0.0) [2]. The registration was performed in two steps: (1) rigid Euler transformation and (2) non-rigid B-spline transformation (Fig.1). The deformation field of the registration was used to calculate the Jacobian matrix. Then, the intradiscal deformation was determined as the determinant of the Jacobian matrix, where a value less than one represents expansion and a value greater than one represents compression. The mean deformation in the whole IVD and for five evenly distributed subregions (anterior-posterior) of the IVD was calculated. The center of mass of the deformation was determined in three directions (left-right, head-feat, anterior-posterior). To select the IVDs and the five subregions, a convolutional neural network implemented in Dragonfly (Vers.2020.1) and a MatLab-based software were used. Mann-Whitney’s U and Kruskal-Wallis H were used (SPSS Inc, Vers.27) to compare global as well as regional deformation measures between groups.
Results
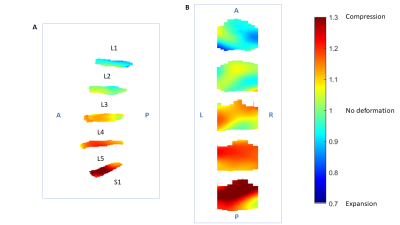
Differences in deformation were found for different spine levels, where IVDs at the lower lumbar levels displayed more compression (p<0.001), even when correcting for degeneration. With the novel imaging method, regional variations in the deformation over the IVD were displayed, with generally more compression at the middle of the IVD and a slightly left asymmetric pattern (Fig.2). IVDs with advanced degeneration (more frequently found in the lower lumbar spine levels) displayed more compression at the posterior region (p=0.035-0.045), even when correcting for spine level. No difference in deformation between patients and controls was found.Discussion
The image-based method, utilizing the deformation field from the registration between MR images during loading and unloading of the spine, displayed load-induced deformation patterns of the IVD both globally and regionally, associated with degeneration and lumbar level. The distribution of the intradiscal deformation in IVDs for different spinal levels and different degeneration grades demonstrates the potential of such new diagnostic tools for the evaluation of the disc pathophysiology in vivo. Another interesting finding was the presence of asymmetries in the deformation pattern over the IVDs, most probably caused by varying disc height across the IVD [3].It is well known that the IVD tissue degenerates during the aging process. When degenerating, the IVD loses its ability to withhold pressure within the nucleus pulposus [4] with a concomitant decrease in stiffness [5-8]. Our data reflected the loss in stiffness in IVDs with high degeneration with more compression for IVDs with pronounced degeneration. Deformation-field MRI could not differentiate between symptomatic patients and asymptomatic controls on a group level but may in combination with conventional MRI markers offer individualized diagnostics.
Conclusion
Using a novel image registration method, it was shown in vivo that the intradiscal deformation depends not only on spine level but also on disc degeneration. This highlights the importance of new diagnostic tools for the evaluation of biomechanical properties of the IVD in vivo. The proposed method offers the possibility to depict and track biomechanical changes non-invasively while characterizing disc structures in detail using MRI.Acknowledgements
The authors would like to acknowledge the Swedish state under the agreement between the Swedish government and the county councils, the ALF-agreement (ALFGBG-792231, 813301, and 772931).References
1. Pfirrmann, C.W., et al., Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine (Phila Pa 1976), 2001. 26(17): p. 1873-8.
2. Klein, S., et al., elastix: a toolbox for intensity-based medical image registration. IEEE Trans Med Imaging, 2010. 29(1): p. 196-205.
3. Byrne, R.M., A.K. Aiyangar, and X. Zhang, A Dynamic Radiographic Imaging Study of Lumbar Intervertebral Disc Morphometry and Deformation In Vivo. Sci Rep, 2019. 9(1): p. 15490.
4. Antoniou, J., et al., The human lumbar intervertebral disc: evidence for changes in the biosynthesis and denaturation of the extracellular matrix with growth, maturation, ageing, and degeneration. J Clin Invest, 1996. 98(4): p. 996-1003.
5. Buckwalter, J.A., Aging and degeneration of the human intervertebral disc. Spine (Phila Pa 1976), 1995. 20(11): p. 1307-14.
6. Nguyen, A.M., et al., Noninvasive quantification of human nucleus pulposus pressure with use of T1rho-weighted magnetic resonance imaging. J Bone Joint Surg Am, 2008. 90(4): p. 796-802.
7. O'Connell, G.D., E.J. Vresilovic, and D.M. Elliott, Human intervertebral disc internal strain in compression: the effect of disc region, loading position, and degeneration. J Orthop Res, 2011. 29(4): p. 547-55.
8. O'Connell, G.D., et al., The effect of nucleotomy and the dependence of degeneration of human intervertebral disc strain in axial compression. Spine (Phila Pa 1976), 2011. 36(21): p. 1765-71.
Figures