0334
Pulmonary vein MRA with reduced sensitivity to off-resonance using optimized contrast preparation1Pediatrics, UT Southwestern Medical Center, Dallas, TX, United States, 2Biomedical Engineering, King's College London, London, United Kingdom
Synopsis
3D bSSFP is the standard for anatomical evaluation of congenital heart disease, but provides suboptimal visualization of the pulmonary veins due to off resonance and flow. Solutions have been proposed to reduce the sensitivity of the bSSFP acquisition to these factors with limited success. However, the T2prep pulse that is routinely applied for bSSFP imaging also likely contributes to pulmonary vein signal loss. In this study, we compare multiple contrast preparation schemes for 3D bSSFP imaging which minimize sensitivity of off-resonance to improve pulmonary vein visualization.
Background
Pulmonary vein (PV) imaging is an important element of congenital heart disease (CHD) evaluation, particularly for anomalous pulmonary veins and PV stenosis. 3D bSSFP is the standard for anatomical evaluation of CHD, but suffers from suboptimal visualization of the PVs due to off-resonance (ΔB0) and rapid blood flow from the lungs (1). Diastolic acquisitions, non-selective refocusing, and bSSFP frequency shifts have been proposed to improve PV blood signal (1), though these are not always effective or clinically desirable. T2 preparation pulses are also applied with bSSFP to increase blood/myocardium contrast. Extended T2prep refocusing intervals increase sensitivity to ΔB0 and flow, and likely contribute to these signal voids (2). The purpose of this study was to evaluate several contrast preparation schemes to improve PV visualization.Methods
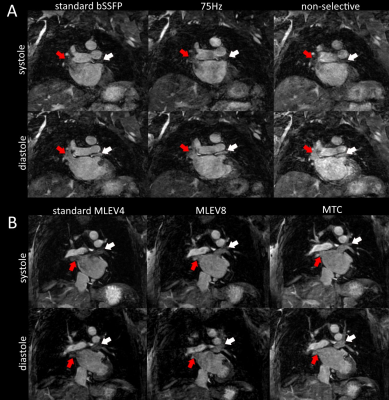
15 patients with CHD and 2 healthy volunteers were scanned on a 1.5T Philips Ingenia. 3D bSSFP datasets were acquired at end-systole in all subjects with a standard T2prep (4 composite refocusing pulses “MLEV4”, TE=50 ms, interval=12.5ms), and TE/TR = 1.7/3.6ms (bSSFP passband = 277Hz).In one volunteer, three previously proposed methods to reduce the sensitivity of bSSFP to ΔB0 and flow were compared to the clinical acquisition: diastolic triggering, non-selective refocusing (TE/TR = 0.97/1.97ms, passband = 512Hz), and a 75Hz bSSFP profile shift (1). In a second volunteer, two pre-pulses that are less sensitive to ΔB0 and flow were compared as an alternate approach to minimize signal loss during systole and diastole: T2prep with shorter refocusing interval (“MLEV8”, TE=50ms, 8 refoc. pulses, interval = 6.25ms) and magnetization transfer contrast (“MTC”, off-resonant, 500 Hz offset, flip angle = 720, 8 repetitions) (3, 4).
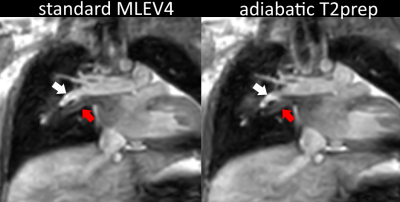
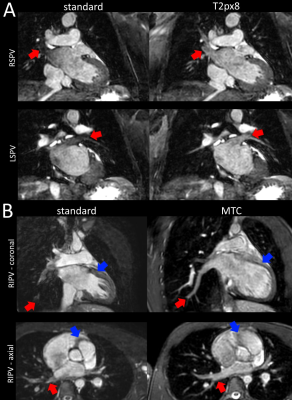
In each patient, the standard MLEV4 pulse was compared to a second 3D bSSFP acquisition with one of the following modified pre-pulses: 1) MLEV8, 2) MTC, or 3) a T2prep with adiabatic refocusing (hyperbolic secant, TE=50ms, 4 refoc. pulses) to reduce the sensitivity of refocusing pulses to ΔB0. 5 patients were included in each of the 3 groups.
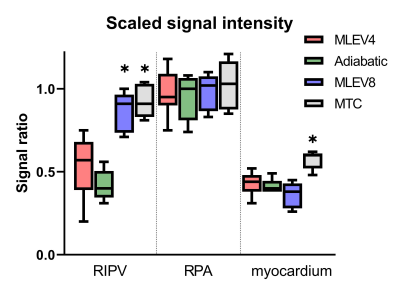
Improvement in PV visualization was evaluated by the RIPV/LV signal ratio, where an ideal ratio of 1 indicates minimal suppression of the veins relative to the intracardiac blood pool. Because the RPA has similar proximity to the lungs but does not suffer from severe signal suppression related to ΔB0, the RPA/RV ratio was reported as a control. The RIPV and RPA signal ratios were calculated using the LV and RV, respectively, to eliminate influence of oxygenation on the signal ratio. The myocardium/RV ratio was also reported as a measure of myocardial suppression.
The proposed pre-pulse modifications increase SAR, but fall within acceptable limits. The average SAR for MLEV4, adiabatic refocusing, MLEV8, and MTC was 1.4, 1.5, 2.0, and 1.9 W/kG.
Results
Figure 1A shows the PVs with standard bSSFP, a 75Hz shift, and non-selective refocusing in one volunteer. These attempts to reduce the bSSFP ΔB0 sensitivity had little effect on the systolic PV blood signal, while the diastolic acquisition provided brighter signal in each case, implying that flow plays a larger role PV suppression than the bSSFP passband. Figure 1B demonstrates improved PV visualization with MLEV8 and MTC compared to the standard T2prep during both systole and diastole in the second volunteer. Figure 2 shows the comparison of MLEV4 and adiabatic refocusing in the same patient. Adiabatic refocusing had no effect on the PV blood signal, suggesting that ineffective refocusing is not a major source of PV signal loss. Figure 3 shows MLEV8 (A) and MTC (B) compared to the standard MLEV4 in two patients. Both pre-pulse modifications significantly improved PV visualization (red arrows). The shorter refocusing interval (MLEV8) reduces the sensitivity of the T2prep pulse to ΔB0 and flow, and increases the PV signal. MTC also provides superior PV visualization, but does not suppress the myocardium as effectively (blue arrows). Figure 4 shows the comparison of RIPV, RPA, and myocardium signal ratios across patients. MLEV8 and MTC significantly increased PV signal compared to the standard MLEV4, while myocardial suppression was less effective with MTC (p<0.05).Discussion
The MLEV4 T2prep pulse with a long refocusing interval plays a significant role in pulmonary vein suppression. Either MLEV8 or MTC pre-pulses can be used to improve visualization of the pulmonary veins. MTC may be more effective restoring vein signal, as it has minimal effect on the blood pool, but does not suppress the myocardium as effectively.Acknowledgements
No acknowledgement found.References
1. Hu P, Stoeck CT, Smink J, Peters DC, Ngo L, Goddu B, Kissinger KV, Goepfert LA, Chan J, Hauser TH. Noncontrast SSFP pulmonary vein magnetic resonance angiography: impact of off‐resonance and flow. Journal of Magnetic Resonance Imaging 2010;32(5):1255-1261.
2. Varghese J, Jin N, Mihai G, Simonetti OP. An improved preparation pulse for quantitative t2 mapping of blood in the cardiac chambers. Journal of Cardiovascular Magnetic Resonance 2015;17(1):1-2.
3. Stoeck CT, Hu P, Peters DC, Kissinger KV, Goddu B, Goepfert L, Ngo L, Manning WJ, Kozerke S, Nezafat RJMrim. Optimization of on‐resonant magnetization transfer contrast in coronary vein MRI. 2010;64(6):1849-1854.
4. Ginami G, Lòpez K, Mukherjee RK, Neji R, Munoz C, Roujol S, Mountney P, Razavi R, Botnar RM, Prieto C. Non‐contrast enhanced simultaneous 3D whole‐heart bright‐blood pulmonary veins visualization and black‐blood quantification of atrial wall thickness. Magnetic resonance in medicine 2019;81(2):1066-1079.
Figures