0330
Feasibility of simultaneous non-contrast coronary MR angiography and vulnerable plaque imaging in acute myocardial infarction1Biomedical Engineering Department, School of Biomedical Engineering and Imaging Sciences, King's College London, London, United Kingdom, 2National Heart and Lung Institute, Imperial College London, London, United Kingdom, 3MR Research Collaborations, Siemens Healthcare Limited, Frimley, United Kingdom, 4School of Biomedical Engineering and Imaging Sciences, King's College London, London, United Kingdom
Synopsis
CMR plaque imaging has the potential to predict future coronary events, but is limited by low spatial-resolution, misregistration artefacts, respiratory motion related image quality degradation and unpredictable acquisition times. Here we clinically evaluate the feasibility of a novel 3D free-breathing, non-rigid motion corrected, non-contrast CMR sequence (iT2prep-BOOST) that enables simultaneous, high-resolution visualisation of the coronary arteries and high-risk plaque features on co-registered bright and black blood images in patients presenting with acute myocardial infarction. We found that iT2prep-BOOST can simultaneously visualise coronary artery stenosis as well as culprit and bystander coronary plaque, as validated against invasive coronary angiography and OCT.
Introduction
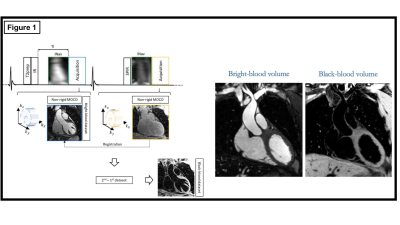
Rupture of an atherosclerotic plaque is the main trigger of myocardial infarction, the leading cause of mortality worldwide. Coronary high-risk plaque identified on cardiovascular magnetic resonance (CMR) is significantly associated with future coronary events, independent of coronary lumen stenosis1. However, CMR plaque imaging is clinically limited by low spatial resolution, misregistration artefacts, respiratory motion related image quality degradation and unpredictable acquisition times. We have recently developed a novel non-rigid motion corrected 3D free-breathing non-contrast CMR sequence that allows for simultaneous high-resolution visualisation of the coronary arteries and high-risk plaque on co-registered bright and black blood images2,3 (Figure 1). Here, we investigate the feasibility of this technique in patients with non-ST-segment elevation myocardial infarction (NSTEMI) and validate it against the gold standard imaging modalities of invasive X-ray coronary angiography and optical coherence tomography (OCT).Methods
The proposed 3D prototype sequence interleaves the acquisition of a T2prep-IR prepared bright-blood dataset with a T1 weighted (T1w) dataset without magnetization preparation3 (iT2prep-BOOST). The bright-blood T2prep-IR dataset enables visualisation of the coronary lumen. Subtraction of the T2prep-IR dataset from the T1w dataset results in a coregistered black-blood dataset that enables visualisation of the coronary vessel wall, thrombus and intraplaque haemorrhage. 2D image-based navigation and respiratory binning enables 2D translational motion correction and 3D non-rigid motion estimation. The final image is obtained using a 3D non-rigid motion compensated iterative SENSE prototype reconstruction for each contrast before subtraction (Figure 1). Reconstruction is implemented inline on the scanner (≈ 5 minutes reconstruction time). The proposed approach enables 100% scan efficiency and predictable scan times. The acquired spatial resolution is 1.2x1.2x1.2 mm3 with 3-fold undersampling and an acquisition time of <15 minutes. The proposed sequence was acquired on a 1.5T MRI scanner (MAGNETOM Aera, Siemens Healthcare, Erlangen, Germany) andcompared against invasive X-ray angiography and intravascular imaging (OCT) in a cohort of 15 patients who presented to our unit with NSTEMI. For visualisation purposes only, a second black-blood image was obtained with phase-sensitive inversion recovery (PSIR)-like reconstruction of the T2prep-IR and T1w datasets which was used for image fusion with the vessel wall (subtraction-based black-blood as described above) dataset.Results
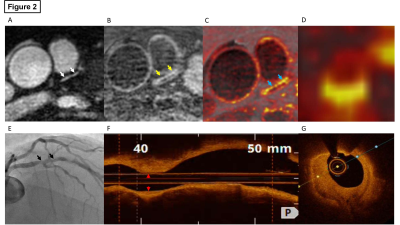
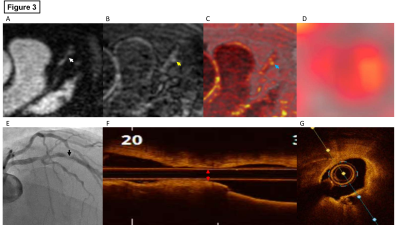
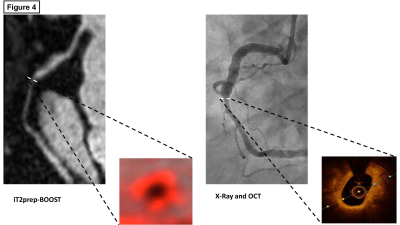
Figures 2, 3 and 4 demonstrate the images of a 54-year-old male patient with no known cardiovascular risk factors. He presented to our heart assessment centre with 24 hours of worsening chest pain. Peak high-sensitivity troponin was elevated at 2173 ng/L. His electrocardiogram demonstrated T wave inversions in the antero-lateral leads. We were able to directly visualise culprit plaque rupture affecting the mid segment of the left anterior descending artery (Figure 3) as well as bystander disease of the proximal to mid left anterior descending artery (Figure 2) using iT2prep-BOOST. Figure 4 demonstrates the images of the same patient’s bystander disease affecting the mid segment of the right coronary artery; directly visualised with iT2prep-BOOST.Conclusion
In summary, the proposed iT2prep-BOOST framework has the potential to simultaneously visualise coronary artery stenosis as well as culprit and bystander coronary plaque in patients presenting with non-ST-segment elevation myocardial infarction.Acknowledgements
No acknowledgement found.References
1. Noguchi T, Kawasaki T, Tanaka A, et al. High-Intensity Signals in Coronary Plaques on Noncontrast T1-Weighted Magnetic Resonance Imaging as a Novel Determinant of Coronary Events. J. Am. Coll. Cardiol. 2014;63:989–999.
2. Ginami G, Neji R, Phinikaridou A, Whitaker J, Botnar RM, Prieto C. Simultaneous bright- and black-blood whole-heart MRI for noncontrast enhanced coronary lumen and thrombus visualization. Magn. Reson. Med. 2018;79:1460–1472.
3. Milotta G, Ginami G, Cruz G, Neji R, Prieto C, Botnar RM. Simultaneous 3D whole‐heart bright‐blood and black blood imaging for cardiovascular anatomy and wall assessment with interleaved T 2 prep‐IR. Magn. Reson. Med. 2019;82:312–325.
Figures