0329
Non-contrast-enhanced free-breathing thoracic MRA using gated REACT at 3T in small children with congenital heart disease1Department of Diagnostic and Interventional Radiology, University Hospital Bonn, Bonn, Germany, 2Department of Diagnostic and Interventional Radiology & Department of Pediatric Cardiology, University Hospital Bonn, Bonn, Germany, 3Philips GmbH Market DACH, Hamburg, Germany
Synopsis
Application of high-resolution 3D MR angiography (MRA) in small children with congenital heart disease (CHD) is challenging and generally requires contrast agent administration. In a cohort of pediatric CHD patients (median age: 4 years), non-contrast-enhanced free-breathing gated 3D mDixon REACT-MRA provided comparable overall image quality to contrast-enhanced free-breathing 3D mDixon steady-state MRA for assessment of the thoracic vasculature. REACT-MRA allowed for accurate and reliable vessel size measurements. Although fat-water separation artifacts were observed, they could be extenuated by reconstruction of in- and out-of-phase images. Gated REACT-MRA allows for a contrast-free assessment of the thoracic vasculature in small children with CHD.
Introduction
Imaging is routinely performed in patients with congenital heart disease (CHD) for initial diagnosis, pre- and postsurgical planning, and lifelong follow-up1. Besides echocardiography, cardiac magnetic resonance (CMR) including MR angiography (MRA) plays a major role in the diagnostic work-up of pediatric patients with CHD, especially for the assessment of vascular structures2. Although macrocyclic gadolinium-based contrast agents have an excellent safety profile, there are concerns regarding its accumulation after serial examinations throughout lifetime3. Main advantages of non-contrast-enhanced CMR examinations include lack of complication risks such as extravasation and allergic reactions, lower examination costs, and facilitation of clinical workflow. Therefore, non-contrast techniques are desirable, especially in children. Yoneyama et al. introduced a novel non-contrast-enhanced flow-independent MRA sequence called REACT (relaxation-enhanced angiography without contrast and triggering) that is based on a T2-prep pulse, a non-volume selective inversion recovery magnetization‑preparation pulse, and 3D dual-echo Dixon method4. First applications for the thoracic vasculature in adults with congenital heart disease showed promising results at 1.5T5. However, imaging of pediatric CHD patients is more challenging due to complex anatomy and small vessel structures. This study aimed to compare non-contrast-enhanced gated 3D REACT-MRA with contrast-enhanced gated 3D mDixon steady state-MRA for the assessment of the thoracic vasculature in pediatric CHD patients at 3T.Methods
The local institutional review board approved this retrospective study and waived informed consent. Patients aged under 10 years with CHD who underwent CMR at 3T including non-contrast-enhanced and contrast-enhanced MRA between April 2021 and July 2021 were identified. Patients were included regardless of the type of CHD or previously performed surgical procedures. The CMR scan protocol was specifically adapted depending on the underlying type of CHD. Single-phase electrocardiogram- and respiratory-gated mDixon steady-state MRA (spatial resolution: 0.45 x 0.45 x 0.70 mm³, compressed SENSE factor 5) was acquired during administration of gadobutrol (0.1 mmol/kg body weight) with slow flow rate. Non-contrast enhanced REACT-MRA was acquired with electrocardiogram- and respiratory-gating before contrast injection (spatial resolution: 0.69 x 0.69 x 1.20 mm³, compressed SENSE factor 6). Water-only, fat-only, in-phase and out-of-phase images were reconstructed for both mDixon-based MRAs. Water-only images were primarily used for image analysis (in the presence of fat-water swapping artifacts, in-phase-images were used). For qualitative analysis image quality of predefined vessels was rated independently by two readers based on a five-point scale (from 1=non-diagnostic to 5=excellent). Vessel diameter measurements of the thoracic vasculature were assessed separately by two readers at predefined landmarks. Blood-to-tissue contrast ratio (regions of interest: ascending aorta and myocardium) was assessed by the first reader. The presence and type of artifact were assessed in consensus by two readers. Paired t test, McNemar test, Wilcoxon signed-rank test, Pearson correlation, Bland-Altman analysis, and intraclass correlation coefficients (ICCs) were used for statistical analysis.Results
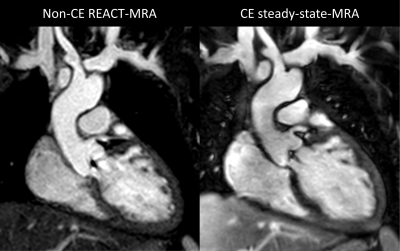
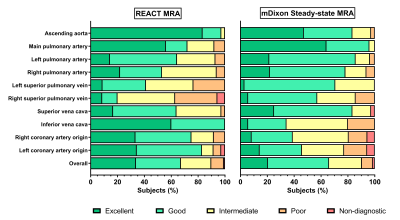
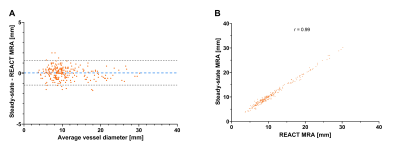
Thirty-six patients with CHD (median age: 4 years, range: 9 months to 9 years; 20 male) were included. REACT-MRA had a longer total acquisition time than steady-state-MRA (4:22±1:44min vs 1:51±0:18min, P<0.001). A representative imaging example of both MRAs is shown in Figure 1. Overall image quality was comparable between REACT- and steady-state MRA (3.9±1.0 vs 3.8±0.9, P=0.018). REACT-MRA provided higher image quality for the ascending aorta (4.8±0.5 vs 4.3±0.8, P<0.001), the inferior vena cava (4.6±0.5 vs 3.2±0.8, P<0.001), and the right (4.0±0.9 vs 3.2±1.0, P<0.001) and left coronary origin (4.1±1.0 vs 3.3±1.1, P=0.001) in comparison to steady-state-MRA (see Figure 2). Image quality of pulmonary veins was intermediate with significant better ratings for steady-state-MRA (e.g., left superior pulmonary vein: 3.3±0.9 vs 3.7±0.5, P=0.005). Image quality of pulmonary arteries was comparable between REACT-MRA and steady-state-MRA (e.g., right pulmonary artery: 3.7±0.9 vs 3.9±0.8, P=0.185). Blood-to-tissue contrast ratio was comparable between REACT-MRA and steady-state-MRA (2.6±0.5 vs 2.7±1.2, P=0.282). Close agreement of vessel diameter measurement was observed between both MRA methods (Pearson r=0.99; bias=0.04±0.61 mm, 95% limits of agreement: -1.17 to 1.24 mm; see Figure 3). REACT- and steady-state-MRA showed good interobserver reproducibility for image quality rating (ICC: 0.87 vs 0.79) and vessel size measurement (ICC: 0.99 vs 0.99). Susceptibility artifacts due to surgical procedures affected both MRAs equally (15/36 patients, 42% for each MRA, P>0.999). Fat-water separation artifacts occurred slightly more frequent on REACT- than steady-state MRA (12/36, 33% vs 5/36, 14%, P=0.109). Flow artifacts were only observed on REACT-MRA (8/36, 22% vs 0/36, 0%, P<0.001) and affected primarily the pulmonary veins (mostly related to high and turbulent flow during diastolic phase) and pulmonary arteries (due to severe pulmonary insufficiency during diastolic phase).Conclusion
Non-contrast-enhanced gated REACT-MRA offers an overall good image quality and allows for accurate and reliable vessel diameter measurements of the thoracic vasculature in pediatric CHD patients. Overall qualitative and quantitative results were comparable to high-resolution contrast-enhanced mDixon steady-state-MRA. Fat-water separation artifacts were observed but can be compensated by reconstruction of in- and out-of-phase images. Specific CHD pathologies associated with high-flow artifacts in the pulmonary vessels may require adjustment of acquisition timing. Because children with CHD require regular CMR early and throughout life, the use of REACT-MRA may be a good alternative to contrast-enhanced MRA techniques and may contribute crucially to a gadolinium-free CMR scanning protocol.Acknowledgements
N/AReferences
1. Triedman JK, Newburger JW. Trends in Congenital Heart Disease: The Next Decade. Circulation 2016;133:2716–2733.
2. Fratz S, Chung T, Greil GF, Samyn MM, Taylor AM, Valsangiacomo Buechel ER et al. Guidelines and protocols for cardiovascular magnetic resonance in children and adults with congenital heart disease: SCMR expert consensus group on congenital heart disease. J Cardiovasc Magn Reson 2013;15:51.
3. Mathur M, Jones JR, Weinreb JC. Gadolinium Deposition and Nephrogenic Systemic Fibrosis: A Radiologist's Primer. Radiographics 2020;40:153–162.
4. Yoneyama M, Zhang S, Hu HH, Le Chong R, Bardo D, Miller JH et al. Free-breathing non-contrast-enhanced flow-independent MR angiography using magnetization-prepared 3D non-balanced dual-echo Dixon method: A feasibility study at 3 Tesla. Magn Reson Imaging 2019;63:137–146.
5. Isaak A, Luetkens JA, Faron A, Endler C, Mesropyan N, Katemann C et al. Free-breathing non-contrast flow-independent cardiovascular magnetic resonance angiography using cardiac gated, magnetization-prepared 3D Dixon method: assessment of thoracic vasculature in congenital heart disease. J Cardiovasc Magn Reson 2021;23:91.
Figures