0317
Real-Time Water Fat Imaging at 0.55T with Spiral Out-In-Out-In Sampling1Ming Hsieh Department of Electrical and Computer Engineering, University of Southern California, Los Angeles, CA, United States
Synopsis
Real-time MRI is a powerful tool to study organ function in a dynamic environment. Many of these regions of interest have both water and fat present, such as the heart and joints. Water/fat separation usually requires multi-echo sequences that utilize chemical shift to distinguish water and fat signals. At 0.55T, the chemical shifts are smaller, making it possible to use long readouts (e.g. spirals) to more efficiently acquire images. Here, we demonstrate spiral out-in-out-in bSSFP imaging combined with region-growing field map estimation for water/fat separation. We demonstrate high quality water/fat separated real-time movies of cardiac function and wrist motion.
Introduction
Real-time MRI has the unique ability to reveal tissue movements and interactions in a non-invasive, radiation-free fashion, and has important diagnostic values in areas that often undergo irregular motions such as the heart and joints1. Recently, 0.55T MRI with high-performance gradients has shown promising results for the heart and speech imaging by leveraging efficient spiral trajectories2,3. Such systems are also desirable for real-time MRI (RT-MRI) due to reduced SAR, reduced susceptibility at air-tissue interfaces, shorter T1 and longer T2*, which will allow for long-readout real-time acquisition with more flexible sequence design and higher acquisition efficiency4.In many regions of interest, both water and fat are present. This results in chemical-shift or blurring artifacts and poses a demand for water/fat separated imaging, which is often done by multi-echo acquisitions. At 0.55T, water and fat have smaller frequency difference, making it possible to use long readouts to efficiently acquire multiple echoes. bSSFP imaging provides high contrast, high SNR efficiency, and is preferred for many RT-MRI applications. RT-MRI with water/fat separation is difficult at high field strengths due to off-resonance and banding artifacts.
In this work, we demonstrate a real-time water/fat imaging by using a bSSFP sequence with a spiral out-in-out-in trajectory at 0.55T. This sequence acquires four images at three echo times within each TR, enabling water/fat separation. High-quality real-time water/fat images were obtained in the heart during free breathing and in the wrist during voluntary movements designed to test joint stability.
Methods
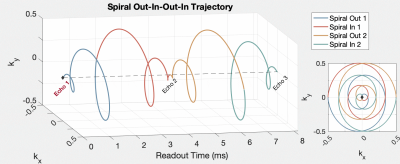
Pulse SequenceFigure 1 illustrates the spiral out-in-out-in bSSFP sequence. A base spiral-out trajectory was first designed. After the first spiral-out, the trajectory continues to sample along the trajectory ($$$k_x(t'),k_y(t')$$$), where $$$k_x(t),k_y(t)$$$ denotes the initial spiral-out trajectory and $$$t'$$$ indicates the reversed time5. The second out-in spiral has a 180o rotation to the first out-in spiral.
Imaging System
Experiments were performed using a whole body 0.55T system (prototype Magnetom Aera, Siemens Healthineers, Erlangen, Germany) equipped with high-performance shielded gradients (45mT/m amplitude, 200T/m/s slew rate). Imaging was performed with RTHawk system (HeartVista Inc., Menlo Park, CA). Data collection used a 6-channel body array and a table-integrated 18-channel spine array.
Cardiac Scans
Four volunteers (1 male, 3 females) were scanned for the heart during free breathing with parameters: voxel size=1.5x1.5x8mm3, Tread=8.14ms, TR=10ms, TE=0.93/5.0/9.07ms, flip angle=80o. ROI shimming was performed for the ventricles, excluding the chest wall.
Wrist Scan
One volunteer was scared during a wrist maneuver, the radial-to-ulnar deviation, relevant to evaluation for dynamic scapholunate instability. The arm was placed above the spine array and below the body-6 array (supported by sandbags), in order to not restrict the range of motion. The parameters were: voxel size=1.4x1.4x8mm3, Tread=8.16ms, TR=10.3ms, TE=1.09/5.17/9.25ms, flip angle=70o. ROI shimming was performed over the base of the wrist and covering all relevant bones and ligaments of the wrist.
Image Reconstruction
Reconstruction was performed using gradient impulse response function predicted trajectories6. Four echo images were reconstructed separately by spatiotemporal constrained reconstruction (STCR)7 at a temporal resolution of 40ms/frame for the heart and 82.4ms/frame for the wrist. Sensitivity maps were estimated from temporally combined first echo image using the Walsh method8. The off-resonance map $$$\varDelta{f}$$$ was estimated using a region-growing iterative method9 frame-by-frame, and then filtered by a [7,7,11] median filter in [x,y,t]. This method assumes a smoothness in $$$\varDelta{f}$$$ and iteratively fit for water, fat, and $$$\varDelta{f}$$$ from echo images.
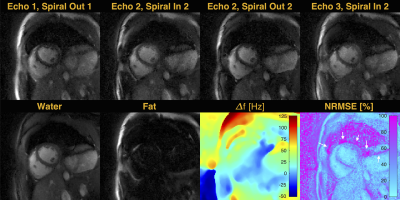
Results
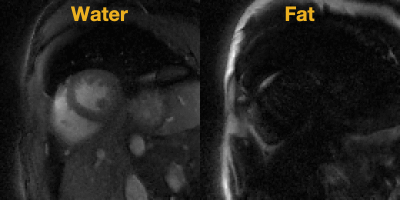
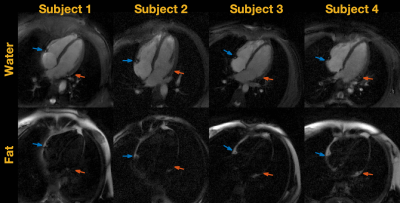
Figure 2 shows fitting results for one representative time frame. The approach achieved good water/fat separation, evidenced in a clear depiction of epicardial fat in the fat-only image and overall low NRMSE. The corresponding free-breathing real-time water/fat movie is shown in Figure 3. The proposed sequence was able to capture detailed structures such as the cross section of the right coronary artery and left circumflex artery in all scans, as shown in Figure 4.Figure 5 shows a water/fat separated real-time movie during radial-to-ulnar deviation maneuver. The fat image depicts the bone marrow clearly as well as all the ligament interval, especially the scapholunate interval that is often important for assessing dynamic wrist instability during the active wrist motion10.
Discussions
In this study, we have demonstrated the feasibility of using a spiral out-in-out-in bSSFP sequence for water/fat separated real-time MRI at 0.55T. The sequence achieved high-quality separation of water and fat in the heart during free breathing and the wrist during voluntary maneuvers. We used a two-step reconstruction approach to obtain water/fat separated images, STCR followed by region-growing $$$\varDelta{f}$$$ estimation. There is potential to improve the performance by directly reconstructing water/fat images such as described in Tan et al.11 and Benkert et al.12Water/fat separation using multiple-echo spirals has been previously demonstrated at higher field strengths13-15. The innovation in this study is the efficient spiral out-in-out-in trajectory that can sample three echoes within one TR and its combination with bSSFP imaging for a substantial boost in SNR efficiency. This is uniquely possible at low field strengths such as 0.55T, and enables real-time characterization of water/fat components in the ROI with high spatio-temporal resolution.
Conclusion
We have demonstrated feasibility of water/fat separation using an innovative bSSFP spiral in-out-in-out sequence at 0.55T. High quality real-time water/fat separation is achieved in the heart and wrist.Acknowledgements
We acknowledge grant support from the National Science Foundation (#1828736) and National Institute of Health (R01-HL130494) and research support from Siemens Healthineers.References
1. Nayak KS, Lim Y, Campbell-Washburn AE, Steeden J. Real-Time Magnetic Resonance Imaging. Journal of Magnetic Resonance Imaging; early view.
2. Restivo MC, Ramasawmy R, Bandettini WP, Herzka DA, Campbell-Washburn AE. Efficient spiral in-out and EPI balanced steady-state free precession cine imaging using a high-performance 0.55T MRI. Magnetic Resonance in Medicine 2020;84(5):2364-2375.
3. Ipshita B, Rajiv R, Matthew CR, Adrienne E C-W. Dynamic speech imaging at 0.55T using single shot spirals for 11ms temporal resolution. ISMRM 2019; Montreal, Canada. p 0440.
4. Campbell-Washburn AE, Ramasawmy R, Restivo MC, Bhattacharya I, Basar B, Herzka DA, Hansen MS, Rogers T, Bandettini WP, McGuirt DR, Mancini C, Grodzki D, Schneider R, Majeed W, Bhat H, Xue H, Moss J, Malayeri AA, Jones EC, Koretsky AP, Kellman P, Chen MY, Lederman RJ, Balaban RS. Opportunities in Interventional and Diagnostic Imaging by Using High-Performance Low-Field-Strength MRI. Radiology 2019;293(2):384-393.
5. Kim DH, Gu M, Spielman DM. Gradient moment compensated magnetic resonance spectroscopic imaging. Magn Reson Med 2009;61(2):457-461.
6. Campbell-Washburn AE, Xue H, Lederman RJ, Faranesh AZ, Hansen MS. Real-time distortion correction of spiral and echo planar images using the gradient system impulse response function. Magn Reson Med 2016;75(6):2278-2285.
7. Adluru G, McGann C, Speier P, Kholmovski EG, Shaaban A, Dibella EV. Acquisition and reconstruction of undersampled radial data for myocardial perfusion magnetic resonance imaging. J Magn Reson Imaging 2009;29(2):466-473.
8. Walsh DO, Gmitro AF, Marcellin MW. Adaptive reconstruction of phased array MR imagery. Magnetic Resonance in Medicine 2000;43(5):682-690.
9. Yu H, Reeder SB, Shimakawa A, Brittain JH, Pelc NJ. Field map estimation with a region growing scheme for iterative 3-point water-fat decomposition. Magn Reson Med 2005;54(4):1032-1039.
10. Shaw CB, Foster BH, Borgese M, Boutin RD, Bateni C, Boonsri P, Bayne CO, Szabo RM, Nayak KS, Chaudhari AJ. Real-time three-dimensional MRI for the assessment of dynamic carpal instability. PLoS One 2019;14(9):e0222704.
11. Tan Z, Voit D, Kollmeier JM, Uecker M, Frahm J. Dynamic water/fat separation and B1 inhomogeneity mapping—joint estimation using undersampled triple-echo multi-spoke radial FLASH. Magn Reson Med 2019;82(3):1000-1011.
12. Benkert T, Feng L, Sodickson DK, Chandarana H, Block KT. Free-breathing volumetric fat/water separation by combining radial sampling, compressed sensing, and parallel imaging. Magn Reson Med 2017;78(2):565-576.
13. Guenthner C, Dillinger H, Boernert P, Kozerke S. Three-Point Dixon Abdominal Water/Fat Separation using a Lower-Field 0.75T MRI. ISMRM 2021; virtual. p 3844.
14. Börnert P, Koken P, Eggers H. Spiral water-fat imaging with integrated off-resonance correction on a clinical scanner. J Magn Reson Imaging 2010;32(5):1262-1267.
15. Wang D, Zwart NR, Pipe JG. Joint water-fat separation and deblurring for spiral imaging. Magn Reson Med 2018;79(6):3218-3228.
Figures