0228
A novel 4D-MRI method enabling real-time image streaming for tumor tracking in radiotherapy1Department of Radiotherapy, University Medical Center Utrecht, Utrecht, Netherlands
Synopsis
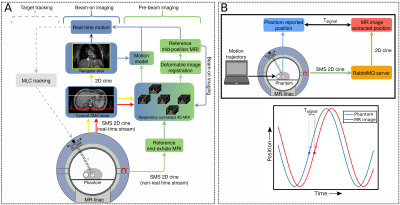
In MR-guided abdominothoracic radiotherapy, fast 2D imaging for MLC tracking and respiratory-correlated 4D imaging for dose accumulation is desirable. We developed a hybrid 2D/4D MRI method for pre-beam and beam-on imaging, which continuously acquires and reconstructs T2w coronal simultaneous multi-slice (SMS) images. Pre-beam 4D-MRIs were used to calculate a 3D mid-position reference image. Beam-on SMS data were used to extract real-time motion using a 4D-based motion model, and continuous 4D-MRIs. Dynamic updating of the 4D-motion model yielded the best real-time motion estimation. The presented hybrid 2D/4D MRI method can potentially facilitate novel MR-guided abdominothoracic radiotherapy workflows.
Introduction
For MR-guided radiotherapy on the MR-linacs, it is desirable to have fast 2D imaging of the target for multileaf collimator (MLC) tracking1 and simultaneously obtain respiratory-correlated 4D-MRIs for dose accumulation. Performing (real-time) 2D and (retrospectively sorted) 4D imaging simultaneously is challenging. Here, we propose a novel hybrid 2D/4D-MRI method by extending our previously developed simultaneous multi-slice (SMS) accelerated 4D-MRI sequence2. Our SMS sequence acquires two coronal slices simultaneously and repeatedly cycles through slice locations over the image volume, covering the full body in the through-plane direction.Methods
All scans were performed on a 1.5 T Unity MR-linac (Elekta AB, Stockholm, SE). To avoid data buffering and lag during the SMS reconstruction we enabled real-time streaming of the SMS data. To this end, we configured the spectrometer to send the k-space data to the Philips reconstructor immediately after acquiring each pair of SMS slices instead of after a package of slices (default). Furthermore, we modified the vendor reconstruction software to start reconstructing a slice as soon as it was received, instead of buffering the data of all slices (default).Experiments with the Quasar MRI4D phantom (ModusQA, London, ON) were performed to determine the latency3 between sampling the center of k-space and receiving the image (Tsignal). The phantom followed a sinusoidal trajectory (A=10 mm, T=4 s) during which SMS images were continuously acquired. The reconstructed SMS images were streamed to a message broker (RabbitMQ) and saved to disk with a timestamp by a client program. The actual phantom positions were streamed to the same client computer such that Tsignal could be determined by calculating the phase shift between the phantom positions and the positions extracted from the image (Figure 1B).
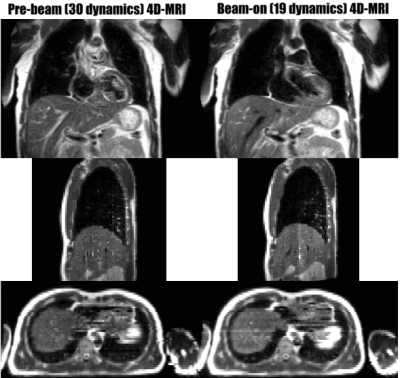
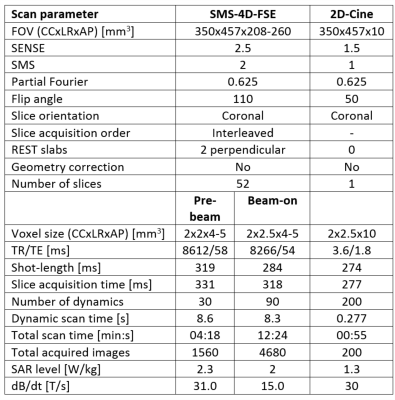
MRI scans of 5 healthy volunteers were acquired. An SMS T2w FSE sequence was acquired covering a stack of 52 slices (350(CC)x457(LR)x208-260(AP) mm3 FOV, Table 1). Per volunteer, two SMS scans were acquired: a ‘pre-beam’ scan (30 dynamics, 4:18 minutes) and a ‘beam-on’ scan (90 dynamics, 12:24 minutes) simulating the two phases of MR-linac treatments. To maximize comfort during beam-on imaging, SAR (heat deposition) and maximum slew rate (acoustic noise) were reduced. The increase in dynamic scan time was compensated by decreasing the in-plane resolution from 2(CC)x2(LR) mm2 to 2x2.5 mm2.
The hybrid 2D/4D image processing workflow is shown in Figure 1A. The pre-beam images were used to create an end-exhale reference volume by registering (normalized cross-correlation) all dynamics to each other in each slice location2. The standard deviation of the cranial-caudal (CC)-shifts relative to this end-exhale volume was determined and used as motion model to account for non-uniform CC-motion across anterior-posterior slice locations in the liver. Using this 4D-based motion model, a unified self-sorting signal was derived representing liver dome CC-motion, and a sorted 4D-MRI was created using amplitude binning. A mid-position volume was derived from the SMS-4D-MRI using deformable image registration4, which served as reference for beam-on imaging.
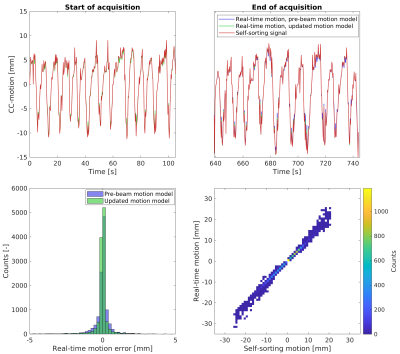
The beam-on SMS data were used for real-time position estimation by rigid registration relative to the pre-beam mid-position image. The 4D-based pre-beam motion model was then applied to convert the CC-motion (per slice) to liver dome motion. Alternatively, the motion model was updated based on the most recent 30 dynamics before use. Next, all beam-on images were used to obtain a self-sorting signal as plausibility check, comparing the real-time motion signals extracted with and without (updated) motion model. In addition, the beam-on data was used to create back-to-back 4D-MRIs while minimizing the acquisition time per beam-on 4D-MRI. To this end, a dynamic inclusion criterion resulting in 10% of missing data in the 4D-MRI was deployed.
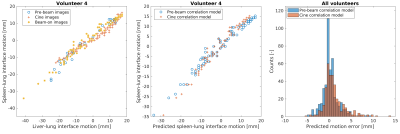
To facilitate real-time motion estimation for lesions beyond the liver dome, a prediction model was developed that estimates lesion motion based on liver-lung interface motion. A prediction model between liver-lung interface motion and spleen-lung interface motion was build using pre-beam images and applied to the liver-lung interface motion in the beam-on images. For comparison, motion was predicted with a prediction model derived from a single-slice 4 Hz coronal 2D cine-MRI acquired in 4 of the volunteers (Table 1). The predicted spleen-lung interface motion was compared to independently extracted (ground-truth) motion.
Results
The signal latency (Tsignal) was 274 ms. Continuously updating the 4D-based pre-beam motion model marginally decreased the mean (SD) error of the real-time motion estimation from -0.01 (1.03) mm to -0.01 (0.81) mm averaged over all volunteers. A time-resolved analysis revealed that updating the motion model slightly improves alignment towards the end of the beam-on acquisition (Figure 2). The dynamic 4D-MRI reconstruction required a median (min-max) inclusion of 28 (18-33) dynamics to fill 90% of the 4D-MRI (Figure 3). The spleen-lung interface motion prediction had a median (min-max) RMSE of 1.9 (0.5-3.0) mm and 1.8 (0.6-4.4) mm for the pre-beam and cine derived prediction models, respectively (Figure 4).Discussion & Conclusion
The presented 2D/4D-MRI workflow demonstrated the potential for accurately extracting real-time motion for MLC tracking in abdominothoracic radiotherapy, while simultaneously reconstructing back-to-back respiratory-correlated 4D-MRIs. To overcome the limitation of not capturing the treatment target with every single slice (as is necessary to achieve volume coverage for the 4D-MRIs), a 4D-based prediction model was used resulting in <2 mm accuracy.Acknowledgements
The authors acknowledge funding by the Dutch Research Council (NWO) through project no. 17515 (BREATHE EASY). We acknowledge research agreements with Elekta AB (Stockholm, Sweden) and Philips Healthcare (Best, The Netherlands).References
1. P Uijtewaal et al. Dosimetric evaluation of MRI‐guided multi‐leaf collimator tracking and trailing for lung stereotactic body radiation therapy. Med Phys. 2021;48(4):1520-1532
2. K Keijnemans et al. Simultaneous multi-slice accelerated 4D-MRI for radiotherapy guidance. Phys Med Biol. 2021;66(9):095014
3. P T S Borman et al. Characterization of imaging latency for real-time MRI-guided radiotherapy. Phys Med Biol. 2018;63(15):155023
4. T N van de Lindt et al. MRI-guided mid-position liver radiotherapy: Validation of image processing and registration steps. Radiother Oncol. 2019;138:132-140
Figures