0222
Highly Accelerated T2 and Diffusion Weighted Imaging of the Prostate by Combining Compressed SENSE, Sparse Sampling and Deep Learning1Institute of Diagnostic and Interventional Radiology, Technical University of Munich, School of Medicine, Munich, Germany, 2Philips GmbH Market DACH, Hamburg, Germany, 3Department of Urology, Technical University of Munich, School of Medicine, Munich, Germany, 4Philips Healthcare, Best, Netherlands
Synopsis
Since prostate MRI is increasingly applied and yet limited by long acquisition times, we prospectively investigated the performance of a novel reconstruction algorithm, combining compressed sensing, parallel imaging and deep learning (C-SENSE AI) in patients with histologically proven prostate cancer. Highly accelerated T2w and DWI sequences were compared to clinical standard of reference T2w and DWI. C-SENSE AI enabled 58% acceleration in T2w imaging and 47% acceleration in DWI of the prostate while obtaining significantly better image quality and tumor detection. C-SENSE AI seems particularly interesting in view of the need for accelerated prostate MRI with preserved high image quality.
Introduction
Prostate Cancer (PCa) is the second most common malignancy in men worldwide, with over 1.2 million new cases per year1. Multiparametric magnetic resonance imaging (mpMRI) outperforms other imaging modalities in visualization of the prostate and is increasingly applied owing to its high significance for tumor detection, preoperative staging and biopsy guidance. Particularly T2-weigthed (T2w) sequences and diffusion-weighted imaging (DWI) play a central role in tumor detection. However, mpMRI is time consuming and especially T2w and DWI contribute to the long examination times. Previous studies on machine learning approaches in prostate MRI have mostly focused on lesion detection and classification2,3. In synopsis of the unprecedented demand for prostate MRI, long acquisition times and the increasing availability of Deep Learning (DL) approaches in MRI, we prospectively evaluated the application of a novel reconstruction approach, combining a deep learning (DL) algorithm with the C-SENSE framework to enable highly accelerated T2w imaging and DWI in patients with histologically proven PCa.Methods
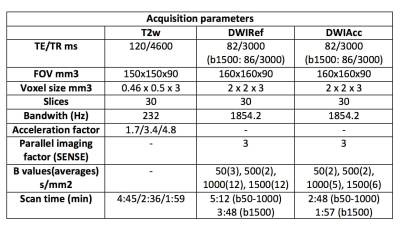
10 healthy volunteers (28.1±3.8 years) and 23 patients (64.4±6.2 years) with histologically proven PCa were prospectively enrolled. T2w datasets were acquired with prospective undersampling using a pseudorandom, density weighted k-space scheme with acceleration factors of 1.7, 3.4 and 4.8. Detailed imaging parameters are displayed in table 1. Subsequently image reconstructions using Compressed SENSE (C-SENSE) and a combination of Compressed SENSE and Deep Learning based Artificial Intelligence (C-SENSE AI) were analyzed. The combination of C-SENSE and Deep Learning was based on the Adaptive-CS-Net presented by Pezzotti et al.4, which combines a Convolutional Neural Network based sparsifying approach with the reconstruction approach of C-SENSE, incorporating prior knowledge such as coil sensitivity distribution and location of the image background and ensures data consistency. In a subset of seven patients a highly accelerated DWI sequence was acquired additionally to the standard of reference DWI with b-values of b50, b500, b1000 and b1500 by reducing the number of signal averages from 17 to 9 for the b50, b500, b1000 scan and from 12 to 6 for the separate b1500 scan, respectively. Both DWI sequences employed a periodic k-space undersampling scheme with a undersampling factor of 3. The standard DWIs were reconstructed using SENSE, the highly accelerated DWIs were reconstruction using C-SENSE AI. Qualitative image comparison (6-point Likert scale: overall image quality, noise, motion artifacts, lesion detection, diagnostic certainty and PI-RADS scores) as well as an objective quantitative image comparison (apparent signal-to-noise ratio (aSNR), apparent contrast-to-noise ratio (aCNR), line profiles at the lesion boundaries and lesion size) were performed by two readers.Results
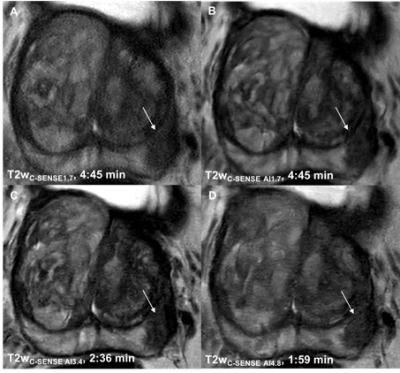
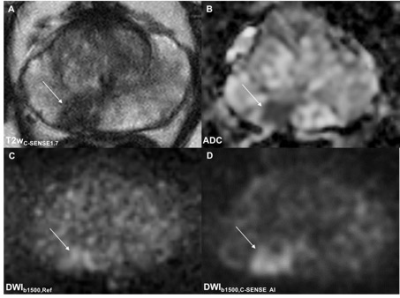
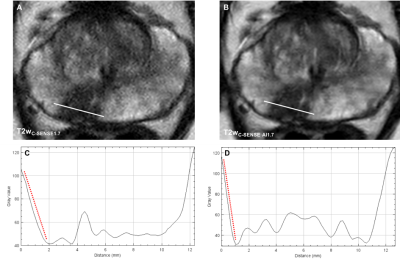
All C-SENSE AI reconstructed images received significantly higher qualitative ratings compared to the C-SENSE standard of reference (Fig. 1, 2). Analysis of the quantitative parameters supported this finding with significantly higher aSNR (p < 0.00001-0.0029) and aCNR (p = 0.00029-0.013). Line profiles demonstrated a significantly steeper signal change at the border of the prostatic lesion and the adjacent normal tissue in the C-SENSE AI reconstructed images (p < 0.00001-0.0036) (Fig. 3) whereas PI-RADS scores (p = 0.81-0.82) and lesion size (p = 0.48-0.5) did not differ.Discussion
Our study is the first to assess the combination of DL, compressed sensing and parallel imaging in a single reconstruction algorithm which is applicable to different image contrasts (i.e. T2w imaging and DWI) in MRI of the prostate. C-SENSE AI reconstructed datasets provided superior image quality, better lesion conspicuity and simultaneously a significant reduction of up to 58% of the scan time compared to C-SENSE and SENSE based image reconstruction. It is of note that increase in image quality, lesion detection and a reduction in motion artifacts was particularly remarkable in a subset of 8 patients who did not receive hyoscine butylbromide which is routinely applied to reduce the occurrence of motion artifacts. Our findings are particularly important regarding the increasing need for prostate MRI due to active surveillance and screening recommendations5,6. Thus, faster and leaner protocols are required meeting the demand of high patient throughput and preserved high image quality.Conclusion
Our study underlines the potential of combining DL and C-SENSE for MRI in patients with prostate cancer. C-SENSE AI enabled higher image quality at accelerated acquisition time for T2w and DWI. Our results seem to be particularly promising and clinically relevant in view of MRI-based screening programs for PCa, patients under active surveillance and the potential implementation of abbreviated biparametric MRI protocols.Acknowledgements
Kilian Weiss and Johannes M. Peeters are employees of Philips Healthcare.References
1. P. Rawla, Epidemiology of Prostate Cancer, World journal of oncology 10(2) (2019) 63-89.
2. P. Schelb, S. Kohl, J.P. Radtke, M. Wiesenfarth, P. Kickingereder, S. Bickelhaupt, T.A. Kuder, A. Stenzinger, M. Hohenfellner, H.P. Schlemmer, K.H. Maier-Hein, D. Bonekamp, Classification of Cancer at Prostate MRI: Deep Learning versus Clinical PI-RADS Assessment, Radiology 293(3) (2019) 607-617.
3. S. Yoo, I. Gujrathi, M.A. Haider, F. Khalvati, Prostate Cancer Detection using Deep Convolutional Neural Networks, Scientific reports 9(1) (2019) 19518.
4. N. Pezzotti, S. Yousefi, M.S. Elmahdy, J.H.F.V. Gemert, C. Schuelke, M. Doneva, T. Nielsen, S. Kastryulin, B.P.F. Lelieveldt, M.J.P.V. Osch, E.D. Weerdt, M. Staring, An Adaptive Intelligence Algorithm for Undersampled Knee MRI Reconstruction, IEEE Access 8 (2020) 204825-204838
5. D. Eldred-Evans, P. Burak, M.J. Connor, E. Day, M. Evans, F. Fiorentino, M. Gammon, F. Hosking-Jervis, N. Klimowska-Nassar, W. McGuire, A.R. Padhani, A.T. Prevost, D. Price, H. Sokhi, H. Tam, M. Winkler, H.U. Ahmed, Population-Based Prostate Cancer Screening With Magnetic Resonance Imaging or Ultrasonography: The IP1-PROSTAGRAM Study, JAMA oncology 7(3) (2021) 395-402.
6. L. Klotz, G. Pond, A. Loblaw, L. Sugar, M. Moussa, D. Berman, T. Van der Kwast, D. Vesprini, L. Milot, M. Kebabdjian, N. Fleshner, S. Ghai, J. Chin, M. Haider, Randomized Study of Systematic Biopsy Versus Magnetic Resonance Imaging and Targeted and Systematic Biopsy in Men on Active Surveillance (ASIST): 2-year Postbiopsy Follow-up, European urology 77(3) (2020) 311-317.
Figures