0213
Use of pCASL MRI to quantify Cerebral Blood Flow and Blood-Brain Barrier Permeability in Patients with Ischemic Stroke1Neurosurgery, THOMAS JEFFERSON UNIVERSITY HOSPITAL, Philadelphia, PA, United States, 2Radiology, THOMAS JEFFERSON UNIVERSITY HOSPITAL, Philadelphia, PA, United States
Synopsis
In this pilot study, we apply diffusion-prepared pseudo-continuous arterial spin labeling (DP-pCASL) non-contrast MRI sequence to patients with anterior circulation ischemic strokes and determine the cerebral blood flow (CBF) and blood-brain barrier (BBB) permeability in the affected vascular territories. When comparing their imaging findings to 24 control hemispheres (12 healthy volunteers), we demonstrated that both the CBF and BBB of the affected MCA territory was significantly lower than the MCA territories in healthy volunteers. Additionally, the BBB permeability in the affected territory appears to be elevated in acute ischemic strokes but decreases in subacute strokes.
Introduction
Cerebrovascular atherosclerosis is the cause of approximately 30% of all ischemic strokes, while it may account up to 56% in certain minorities1,2. Despite receiving the standard-of-care medical and surgical treatment, 20% of patients will have a recurrent stroke within 5 years of treatment with 3.7% of them being fatal3. Carotid atherosclerosis that extends intracranially further raises the risk of recurrent stroke to 23% within the first year4. The high rates of stroke underscore the pressing need to better understand the hemodynamics underlying stroke occurrence. In our pilot study, we utilize the novel diffusion-prepared pseudo-continuous arterial spin labeling (DP-pCASL) non-contrast MRI sequence that generates cerebral blood flow (CBF) and blood-brain barrier (BBB) permeability maps of the affected vascular territory in patients with anterior circulation strokes5.Methods
The study protocol was approved by the University Institutional Review Board. We conducted a prospective controlled study of patients with acute ischemic stroke treated at a comprehensive stroke center from September, 2021 to October, 2021. Patients underwent non-contrast MRI of the brain for evaluation of their stroke burden as well as the investigational DP- pCASL MRI (Siemens 3T, 64-channel coil, voxel size 3.5x3.5x8.0, TR 4.2s, bolus duration 0.7s, inversion time 1.8s, M0-PLD at 2s, TA 10 minutes). The control arm included healthy adults without any cerebrovascular history that underwent high resolution T1, T2 and DP-pCASL imaging. Post-processing was performed using the water exchange rate quantification toolbox (Shao et al, 2019) to generate CBF and BBB permeability maps. Registration was performed using the ANT toolbox using syn-based registration to register the MNI space to each subject’s T1 scan. The registered MNI scan was then registered to the M0 ASL scan of the patient using the FLIRT toolbox (FSL) using linear rigid registration. Finally, vascular masks that are co-registered to the MNI space were overlaid over the CBF and BBB maps and the mean intensity of each vascular territory was calculated using ITK-SNAP. The average CBF and BBB values for the affected vascular territory (anterior cerebral and middle cerebral artery) were compared to the contralateral territory as well as the controls. Each hemisphere of the participants from the control arm was considered independently. The average CBF and BBB values of each vascular territory were divided over the subject’s whole brain average value to control for baseline variability in brain perfusion. Data are presented as median and interquartile range for continuous variables that are not normally distributed and as frequency for categorical variables. The Mann-Whitney test was performed for continuous variables that did not conform to normal distribution. Statistical analysis was carried out with IBM SPSS.Results
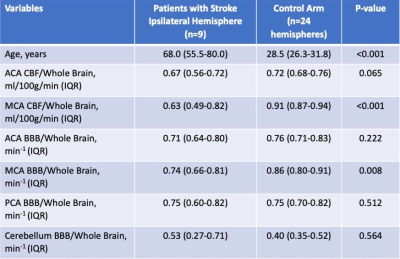
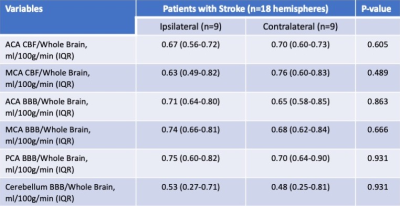
A total of 9 patients with acute ischemic stroke and 12 volunteers were enrolled in our study, resulting in analysis of 9 hemispheres affected with stroke, 9 contralateral unaffected hemispheres, and 24 control hemispheres. The median age of the investigational and control arms were 68.0 (IQR: 55.5-80.0) and 28.5 (26.3-31.8, p<0.001) respectively. The imaging was obtained at a median of 39.1 (IQR: 25.7-60.5) hours from stroke symptom onset. The whole brain average CBF and BBB were 28.8ml/100g/min (IQR:25.6-33.5) and 106.3 min-1 (IQR:82.7-109.3) respectively in the investigational arm, and 47.8ml/100g/min (IQR:42.9-52.4) and 130.8 min-1 (IQR:111.9-140.5) respectively for the control arm. When comparing to controls, the affected MCA CBF/ whole brain CBF was significantly lower than the controls: 0.6 (0.49-0.82) vs. 0.91 (0.87-0.94, p<0.001). The affected MCA CBF/whole Brain was also lower than the contralateral MCA territory in the same patients but did not achieve statistical significance (0.76; IQR: 0.60-0.73; p=0.489). The affected MCA BBB/whole brain BBB was also significantly lower than in controls: 0.74 (0.66-0.81) vs. 0.86 (0.80-0.91; p=0.008), but this relationship did not achieve statistical significance against the contralateral territory (p=0.666). Our detailed results are displayed in Tables 1 and 2.Discussion
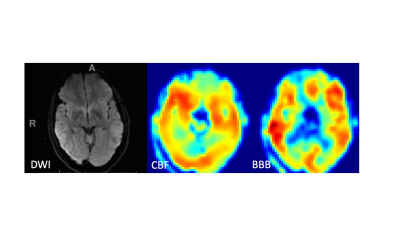
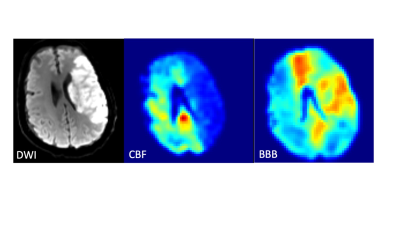
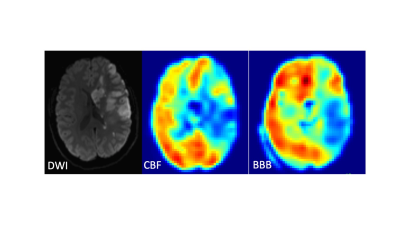
Our pilot study demonstrates the feasibility of using DP-pCASL to quantify CBF and BBB permeability in patients with ischemic stroke. Figures 1 shows the DWI and DP-pCASL findings of a healthy control, while figures 2 and 3 are from patients with acute and subacute strokes respectively. CBF is decreased at the infarcted territory of both patients, however the BBB permeability is elevated at the infarcted area in Figure 2 but decreased in Figure 3. These findings corroborate the effect of ischemic strokes on CBF and BBB without the need for gadolinium. This sequence can help physicians to determine the optimal timing for initiating anti-thrombotic medications, endovascular stenting or carotid endarterectomy to prevent secondary stroke while minimizing the risk of hemorrhagic conversion. While our findings are promising, our small sample size is the major limitation and further investigation is necessary to corroborate DP-pCASL’s clinical utility.Conclusion
The use of DP-pCASL in patients with ischemic stroke demonstrates significantly lower CBF and BBB permeability in the affected territories when compared to controls. Our findings warrant larger-scale studies to assess the utility of DP-pCASL in guiding the timing of further medical and surgical treatments for patients with ischemic stroke.Acknowledgements
No acknowledgement found.References
1. Arenillas JF. Intracranial atherosclerosis: Current concepts. Stroke. 2011;42(1 Suppl):S20-3. doi: 10.1161/STROKEAHA.110.597278 [doi].
2. Gorelick PB, Wong KS, Bae HJ, Pandey DK. Large artery intracranial occlusive disease: A large worldwide burden but a relatively neglected frontier. Stroke. 2008;39(8):2396-2399. doi: 10.1161/STROKEAHA.107.505776 [doi].
3. Dhamoon MS, Sciacca RR, Rundek T, Sacco RL, Elkind MS. Recurrent stroke and cardiac risks after first ischemic stroke: The northern manhattan study. Neurology. 2006;66(5):641-646. doi: 66/5/641 [pii].
4. Kasner SE, Chimowitz MI, Lynn MJ, et al. Predictors of ischemic stroke in the territory of a symptomatic intracranial arterial stenosis. Circulation. 2006;113(4):555-563. doi: CIRCULATIONAHA.105.578229 [pii].
5. Shao X, Ma SJ, Casey M, D'Orazio L, Ringman JM, Wang DJJ. Mapping water exchange across the blood-brain barrier using 3D diffusion-prepared arterial spin labeled perfusion MRI. Magn Reson Med. 2019;81(5):3065-3079. doi: 10.1002/mrm.27632 [doi]
Figures