0209
A prospective patient study using pseudocontinuous Arterial Spin Labeling to detect pulmonary embolism: preliminary results of an ongoing study1Diagnostic and Interventional Radiology, University Hospital of Tübingen, Tübingen, Germany, 2High-Field MR Center, Max Planck Institute for Biological Cybernetics, Tübingen, Germany, 3Section on Experimental Radiology, University Hospital of Tübingen, Tübingen, Germany, 4Neuroradiology, University Hospital of Mainz, Mainz, Germany
Synopsis
We present preliminary results of a prospective study of 96 patients examined with pCASL-MRI of the lung with suspected pulmonary embolism. pCASL-MRI of the lung was acquired in a 1.5T scanner by labeling the pulmonary trunk during systole. Coronal, sagittal and axial images were acquired using a fast bSSFP sequence. Additionally, a mulit-slice coronal bSSFP imaging the whole lung was performed. Two blinded readers evaluated MR-images to detect pulmonary embolism and noted the diagnostic confidence (5=very good). Compared to CT, sensitivity and specificity were 0.971 and 0.951. The median diagnostic confidence was 5 in both readers (kappa 0.739).
Introduction
Acute pulmonary embolism (PE) requires immediate and precise diagnostic imaging to confirm the diagnosis and assess the severity of pulmonary perfusion defects. Contrast-enhanced computed tomography (ceCT) is the reference standard and detects PE as filling defects in pulmonary arteries. Recently, we presented pseudocontinuous Arterial Spin Labeling (PCASL) with balanced steady-State Free-Precession (bSSFP) readout at 1.5T as a non-invasive technique to image pulmonary perfusion even under free breathing conditions1. However, the performance of ASL imaging of the lung in clinical routine remains unclear. We present the first preliminary results of a prospective study aimed at determining the diagnostic performance of PCASL imaging in direct comparison to ceCT in 96 patients with suspected PE.Material and Methods
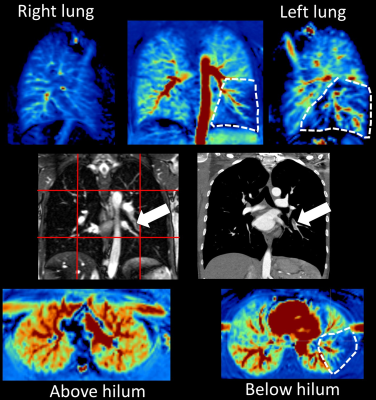
Examination: This study was approved by the local ethics committee and is registered at the German Clinical Trials Register (DRKS00023599). Inclusion criteria: adult patients with clinically suspected PE examined in ceCT within the last 72h, haemodynamically stable, written informed consent. Exclusion criteria: >110 bpm, mmHg syst. <100, typical contraindications for MRI. Assuming a prevalence of PE of 0.32, the required sample size is 97 participants for a two-sided 95% sensitivity confidence interval with a width of 0.2. PCASL MRI was performed with a 1.5T MR scanner (MAGNETOM Avantofit, Siemens Healthcare, Erlangen, Germany) under free breathing conditions. The labeling plane was placed perpendicular to the pulmonary trunk and the pulse train was triggered by the ECG signal during the systolic period (labeling duration 300 ms). Following a post-labeling delay of 1000 ms, coronal, sagittal and axial images were acquired using a fast bSSFP sequence (Fig. 1) with following parameters: TR 2.1 ms, TE 0.9 ms, flip angle 70°, FoV 480×480 mm2, ST 20 mm, matrix 144×192, BW 1240 Hz/Pixel. Additionally, a multi-slice coronal bSSFP imaging of the whole lungs was performed as follows: TR 390.6 ms, TE 1.35 ms, flip angle 80°, FoV 480×480 mm2, ST 4 mm, matrix 210×320, BW 975 Hz/Pixel, iPAT 2. Total examination time ranged from 15-20 min.Analysis: Registration of perfusion data was conducted by the open-source toolbox elastix3,4 using an in-house developed MATLAB® (The Mathworks, Natick, MA) script as decribed in the previous work1. A blinded reading of PCASL and multi-slice bSSFP images was performed by two senior radiologists with several years of experience in MRI. Perfusion defects suspected for PE were noted and the diagnostic confidence was rated using a likert scale (5 is very high).
Results
From 11/2020 till 11/2021, 96 of 97 patients were included to the study. In 31 patients, PE was diagnosed in ceCT, an example is given in Fig. 2. PCASL MRI could be performed successfully in all patients. Both readers rated 1 patient false negatively and 3 patients false positively in PCASL MRI. Median diagnostic confidence was rated as 5 in both readers (inter-rater reliability kappa was 0.739). Sensitivity and specificity were 0.971 and 0.951.Discussion
ceCT is the standard of care in clinical routine for the detection of PE, but requires intravenous contrast agent to detect blood clots in the pulmonary arteries which can cause life-threatening allergic reactions or nephropathy. Radiation exposure should be avoided in young or pregnant patients which can lead to a diagnostic dilemma in clinically unclear cases. Moreover, ceCT can not reveal the resulting functional information, i.e. the perfusion defects in lung parenchyma. In the present study, we could demonstrate that PCASL-MRI of the lung can be applied in a clinical setting even under free breathing conditions in a large patient cohort. Together with multi-slice bSSFPimaging of the whole lung, PE could reliably be detected with a low rate of false positives/negatives. These cases need to be evaluated more in detail in the following data evaluation. The diagnostic confidence was very high in both readers which a good inter-rater reliability. This underlines the potential of PCASL MRI of the lung for clinical questions in the future.Acknowledgements
No acknowledgement found.References
1. Seith F, Pohmann R, Schwartz M, et al. Imaging Pulmonary Blood Flow Using Pseudocontinuous Arterial Spin Labeling (PCASL) With Balanced Steady-State Free-Precession (bSSFP) Readout at 1.5T. J Magn Reson Imaging. 2020;52(6):1767-1782.
2. Penaloza A, Kline J, .Verschuren F, et al. European and American suspected and confirmed pulmonary embolism populations: comparison and analysis. JThromb and Haemost 2012;10:375-381.
3. Klein S, Staring M, Murphy K, et al. Elastix: a toolbox for intensity based medical image registration. IEEE Trans Med Imaging. 2010;29(1):196-205.
4. Shamonin DP, Bron EE, Lelieveldt BPF, et al. Fast parallel image registration on CPU and GPU for diagnostic classification of Alzheimer’s disease. Front Neuroinform. 2014;7:50.
Figures