0188
BraCoil – a wearable one-size-fits-all breast coil for 3 T MR mammography1High Field MR Center, Center for Medical Physics and Biomedical Engineering, Medical University of Vienna, Vienna, Austria, 2IADI, Inserm, Université de Lorraine, Nancy, France, 3Laboratoire d’Imagerie Biomédicale Multimodale Paris Saclay (BioMaps), CEA, CNRS, Inserm, Université Paris-Saclay, Paris, France
Synopsis
In this work, we present a new approach for MR mammography with a wearable light-weight coil array (“BraCoil”) covering both breasts and the sentinel axillary lymph nodes. The coil can be worn like a vest over a T-shirt and used either in prone or supine position. The presented design might be able to overcome numerous shortcomings of the current state-of -the-art in breast imaging by improving sensitivity, comfort and intimacy, shortening measurement time and may thereby eventually enable large-scale breast cancer screening without ionizing radiation.
Introduction
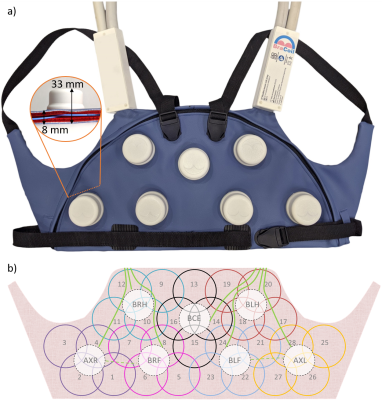
MR mammography is typically performed with RF receive coils integrated into rigid cup-shaped molds and with the patient lying with exposed breasts on their front (prone1) with her arms above the head. The cup size is chosen to accomodate a significant fraction of the patient population. However, the loading of the RF coil can be suboptimal for small breasts, leading to reduced sensitivity, whereas the cup size can also be insufficient to accommodate the entire breast in other patients. MR technologists consider patient positioning complicated, and patients find the imaging position uncomfortable. The gravitational tissue deformation between prone MRI and most other modalities (e.g. ultrasound) and surgery, which are performed with the patients lying on their back (supine), complicate diagnosis and treatment2. Breast MRI in supine position3 yields the same diagnostic value as examinations in prone position4 and facilitates image fusion to supine ultrasound5. In the diagnosis of breast cancer, assessment of the axillary sentinel lymph nodes is important, however, in most setups they are not covered by the RF coil. All these problems underline the need for technological advances to improve patient comfort, image quality, and consistency with other imaging modalities and therapeutic interventions. In this work, we present a new approach for MR mammography with a wearable vest-like coil array (“BraCoil”) that can be used either in prone or supine position with the arms next to the body (Fig.1).Methods
BraCoil is a receive-only array of 28 flexible single-gap coaxial coil elements6, arranged in seven 4-channel modules covering both breasts and axillae (Fig.2). Each module7 contains 4 overlapping elements arranged as a diamond-shaped part of a classical hexagonal array layout. A 3D-printed screwable round housing encloses the module’s interfacing electronics arranged on 2 stacked PCBs including fuses, tuning, matching, active detuning, lattice baluns, and preamplifiers. The bottom and top parts of the housing clamp together the artificial leather cover layers and inner cushion layers (Fig.2a). Detuning bias is implemented module-wise, and the bias lines are bundled with the four receive cables. These bundles are routed (<23cm length) between the cushion layers to bilateral shoulder interface boxes containing floating cable traps8 and a cable strain relief for two Siemens system cables one each side. The BraCoil can be opened for maintenance by unscrewing the housings and opening a semi-circular plastic zipper in the textile. It is fitted to the subject’s body by two adjustable shoulder belts and a waist belt. Bench tests were performed on a network analyzer (Keysight Technologies E5071C, Santa Rosa, USA). S-parameters (matching and coupling) were measured with the coil form-fitted to a phantom. Active detuning efficiency ΔS21 was obtained from double loop probe measurements. All MR scans were acquired on a 3T MR scanner (Prisma Fit, Siemens Healthineers, Erlangen, Germany) on a 25-liter torso phantom (filled with acrylic gel, σ= 0.60S/m, ε=62) with strap-on silicone breasts (“C-cup realistic strap-on breast”, Vollence). Flip-angle maps9 were acquired with the MR system’s body coil with and without BraCoil present to calculate B1+-ratio maps determining detuning efficiency. The noise correlation matrix10 was calculated from a noise-only scan. Sagittal and transversal 2DGRE images were acquired.Results
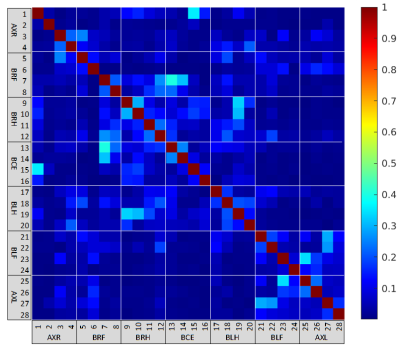
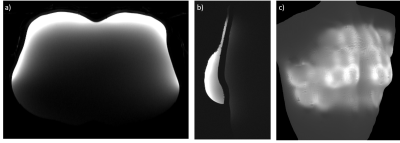
In Fig.3 the S-parameter matrix is shown. The average matching is -18.5dB (<-11.2dB), coupling is on average -39.5dB overall and -20.2dB within the modules (<-12.3dB). Detuning efficiency is on average 28.9dB (>21dB). The change in the body coil’s B1+-field is below 10% around 2cm inside the phantom. The noise correlation matrix can be seen in Fig.4, average correlation is 0.07 (max.0.4). MR phantom images are shown in Fig.5. A companion abstract by Nohava et al. demonstrates strongly improved SNR and parallel imaging performance in comparison to commercial coils. The coil weight on the subject (excluding system cables, since they are supported by the patient bed) is ~1.5kg. The sensitive area is approximately 55x20cm².Discussion
The presented phantom images show that the coverage of the BraCoil nicely fits the desired sensitive area in the breast. With the flexible vest approach, a much more natural breast shape compared to standard breast MR imaging can be achieved. The coil can be used both in supine and prone position. While free-breathing supine imaging is preferable for comfort and a similar breast shape to ultrasound or surgery, breathing motion is a limiting factor, which might be overcome by the combination of motion sensors together with a reconstruction-based correction method11. In prone positioning, the breast is flattened by the weight of the subject, but motion is not an issue. Undoubtedly the shape will differ from the supine position, but is still much more similar than the standard “hanging breast” setup.A patent is filed12, the regulatory steps for in vivo usage are currently underway, and first in vivo data can be expected after Ethics approval (early 2022).
Conclusion
In this abstract we present the main design features and show that the coil performs as intended. The flexible vest-like approach of the presented breast coil is both comfortable and robust and has the potential to strongly improve image quality in MR mammography.Acknowledgements
This work was funded by a joint Austrian/French grant (Austrian Science Fund FWF Nr. I-3618/Agence Nationale de Recherche ANR-17-CE19-0022) “BRACOIL“ and the Anniversary Fund of the Oesterreichische Nationalbank Nr. 17980 “FlexShim“.References
1. Nnewihe, A. N. et al. Custom-fitted 16-channel bilateral breast coil for bidirectional parallel imaging. Magn. Reson. Med. 66, 281–289 (2011).
2. Telegrafo, M., Rella, L., Stabile Ianora, A. A., Angelelli, G. & Moschetta, M. Supine breast US: how to correlate breast lesions from prone MRI. Br. J. Radiol. 89, 20150497 (2016).
3. Fausto, A. et al. Feasibility, Image Quality and Clinical Evaluation of Contrast-Enhanced Breast MRI Performed in a Supine Position Compared to the Standard Prone Position. Cancers 12, (2020).
4. Siegler, P., Holloway, C. M. B., Causer, P., Thevathasan, G. & Plewes, D. B. Supine breast MRI. J. Magn. Reson. Imaging 34, 1212–1217 (2011).
5. Yoon, G. Y. et al. Feasibility of supine MRI (Magnetic Resonance Imaging)-navigated ultrasound in breast cancer patients. Asian J. Surg. 43, 787–794 (2020).
6. Zhang, B., Sodickson, D. K. & Cloos, M. A. A high-impedance detector-array glove for magnetic resonance imaging of the hand. Nat Biomed Eng 2, 570–577 (2018).
7. Obermann, M., Roat, S. & Laistler, E. Coaxial coil modules as building blocks of individually arranged receive-only coil arrays. in Proc. Intl. Soc. Mag. Reson. Med. 29 (2021) 1610.
8. Seeber, D. A., Jevtic, J. & Menon, A. Floating shield current suppression trap. Concepts in Magnetic Resonance vol. 21B 26–31 (2004).
9. Chung, S., Kim, D., Breton, E. & Axel, L. Rapid B1+ mapping using a preconditioning RF pulse with TurboFLASH readout. Magn. Reson. Med. 64, 439–446 (2010).
10. Robson, P. M. et al. Comprehensive quantification of signal-to-noise ratio and g-factor for image-based and k-space-based parallel imaging reconstructions. Magn. Reson. Med. 60, 895–907 (2008).
11. Chen, B. et al. Design and Validation of a Novel MR-Compatible Sensor for Respiratory Motion Modeling and Correction. IEEE Trans. Biomed. Eng. 64, 123–133 (2017).
12. Laistler, E., Obermann, M., Nohava, L., Roat, S. Coil module for magnetic resonance imaging applications. Patent. Application number EP21020242.0 - 1126 (2021).
Figures