0151
Silicone Implant and Fibrous Capsule Assessment Based on Water-Fat-Silicone Images from a Chemical Shift Encoding-Based Species Separation1Technical University of Munich, Munich, Germany
Synopsis
With continuously rising breast augmentation procedures worldwide, there is an increasing clinical need for an early and accurate detection of implant complications. In clinical practice, silicone implants are mainly visualized by silicone-only acquisitions which can be limited by a low signal-to-noise ratio and poor resolution. The present work proposes chemical shift encoding-based multi-echo gradient-echo imaging in combination with a robust graph-cuts-based water-fat-silicone separation. The resulting multi-contrast imaging at high isotropic resolution enables a more precise delineation of the implant capsule and a better evaluation of the implant’s integrity compared to conventional silicone-only acquisition.
Introduction
In 2019, almost 1.8 million breast augmentation procedures including aesthetic surgery and breast reconstruction after cancer therapy were performed worldwide (1). Silicone breast implants presenting 80% of all clinically applied implants are the most utilized augmentation material due to their biocompatibility and physical stability (1). However, long term employment has revealed early and late onset complications such as capsular contracture, rupture or implant associated large cell lymphoma, that are often too discreet to detect in clinical examination (2). The risk of ruptures drastically increases after 6-8 years of implantation with rupture rates of up to 35% after primary breast reconstruction (3). Regarding the poor clinical detection rate and the severity of undiagnosed complications, MRI presents a sensitive alternative to assess the integrity of silicone implants. In clinical routine, T2-weighted turbo spin echo acquisitions combining frequency-selective water suppression and short tau inversion recovery (STIR) for fat suppression or double inversion recovery (DIR) for water and fat suppression are primarily used to generate silicone-only images (4, 5). However, these silicone-only images present several inconveniences including a low signal-to-noise ratio (SNR) efficiency and a consecutively coarse resolution, a considerable motion sensitivity and a long scan time (6). Recently, previous works have developed an algorithm for the joint estimation of water-, fat- and silicone-separated images in chemical shift encoding-based (CSE-)imaging to overcome the poor image resolution and unfavorable SNR (7). The present study aims to compare the quality and applicability of the new water-fat-silicone separation method compared to the most frequently used silicone-only method in the clinical setting.Methods
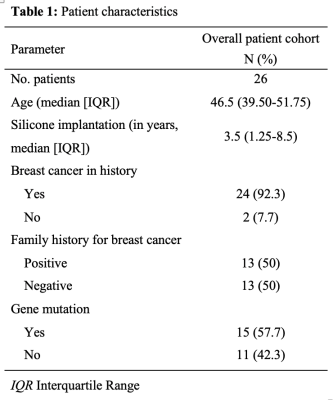
In this retrospective study, 26 women with uni- or bilateral silicone implants were subjected to 3T MRI (Philips Ingenia, Best, Netherlands) between January to September 2021 (Table 1). MRI included (a) silicone-only T2-weighted turbo spin echo DIR acquisition with TE=65ms, TR=15.7s, FOV=220x382.6x192.4mm³, scan time 3:08min, and (b) CSE-imaging based on a monopolar time-interleaved multi-echo gradient-echo sequence acquiring 6 echoes in two TRs with TE=1.58ms, ∆TE=1.28ms, FOV=220x382.6x192.4mm³, scan time 4:15min (8). DIR magnitude and real images were extracted. The gradient echo data was processed with a custom reconstruction and post-processing pipeline based on multiple connected graph-cut layers with different properties solving the B0 field-map. The spatial resolution was increased for subsequent graph-cut layers starting from a coarse signal resolution to conclude with a high-resolution field-map. Water-, fat- and silicone-separated images were calculated based on the field-map and corrected for a fitted estimate. The water-fat-silicone CSE-images were evaluated using a clinically established rating which included the assessment of the differentiability of the silicone implant to the surrounding breast tissue, the visibility and contouring of the adjacent fibrous capsule as well as the accuracy of intralesional folds. Secondly, these parameters were directly compared to the silicone-only imaging results. The rating was expressed in increasing quality from 1-5 and was conducted by three experienced radiologists blinded to the study purpose. The inter-reader reliability was assessed using Cohen’s kappa. In addition, an apparent contrast-to-noise (aCNR) was determined by placing a ROI into the silicone implant and adjacent fat tissue as a reference. Statistical analyses were performed using R (R Foundation for Statistical Computing, 1.3.1056, 2020).Results
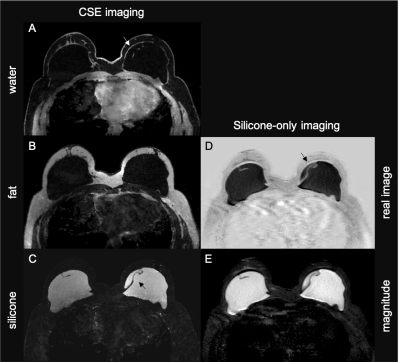
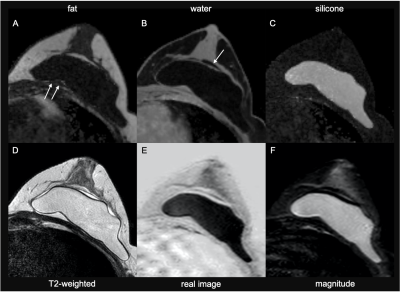
The average quality of water-fat-silicone images from CSE imaging was assessed as 4 (good). Out of 26 silicone assessments, two examinations were evaluated as poor due to overlaying motion artefacts. In the majority of images, a concise delineation of the silicone implant was achieved in silicone-separated CSE imaging along with a precise visualization of the thin surrounding fibrous capsule that was not distinguishable in silicone-only imaging (Fig.1). The inter-reader reliability between the three radiologists in the image quality ratings was categorized as “substantial” (k=0.7). The aCNR was significantly higher in the silicone CSE-based images compared to silicone-only imaging (p<0.0001). This finding is congruent with a better differentiability and more precise depiction of the integrity of the silicone implant in CSE imaging compared to silicone-only imaging. In contrast, neither in CSE imaging nor in silicone-only imaging, seroma adjacent to the silicone implant was sufficiently displayable (Fig.2).Discussion
In clinical practice in MRI, silicone implants are mainly visualized with T2-weighted turbo spin echo STIR/DIR acquisitions which are limited by a low SNR efficiency and poor resolution and therefore render the diagnosis of complications such as rupture and capsule contraction challenging. The present work uses intrinsically co-registered water-, fat- and silicone-separated gradient-echo images generating a high isotropic resolution and therefore an increased contrast of silicone to the surrounding tissue. This allows for a precise delineation of the fine fibrous capsule which naturally forms around the implants but often leads to an underdiagnosed capsule contraction (9). Furthermore, CSE imaging allows for a short scanning time which facilitates the implementation into clinical routine MR examination.Conclusion
CSE imaging enables the acquisition of water-, fat- and silicone-separated images which enables a simultaneous silicone implant and surrounding fibrous capsule assessment. The improved differentiability and delineation of the silicone implant and especially the precise visualization of the surrounding fibrous capsule compared to silicone-only imaging may provide clinicians with a valuable tool for an accurate evaluation of the integrity of silicone implants and an early detection of potential complications.Acknowledgements
We would like to thank the technical assistants to conduct the MRIs.References
1. Surgery ISoAP. ISAPS International Survey on Aesthetic/Cosmetic Procedures performed in 2019. 2019 [Available from: https://www.isaps.org/wp-content/uploads/2020/12/Global-Survey-2019.pdf.
2. Kricheldorff J, Fallenberg EM, Solbach C, Gerber-Schafer C, Rancso C, Fritschen UV. Breast Implant-Associated Lymphoma. Dtsch Arztebl Int. 2018;115(38):628-35. 10.3238/arztebl.2018.06283.
3. Hillard C, Fowler JD, Barta R, Cunningham B. Silicone breast implant rupture: a review. Gland Surg. 2017;6(2):163-8. 10.21037/gs.2016.09.124.
4. Monticciolo DL, Nelson RC, Dixon WT, Bostwick J, 3rd, Mukundan S, Hester TR. MR detection of leakage from silicone breast implants: value of a silicone-selective pulse sequence. AJR Am J Roentgenol. 1994;163(1):51-6. 10.2214/ajr.163.1.80102475.
5. Mukundan S, Jr., Dixon WT, Kruse BD, Monticciolo DL, Nelson RC. MR imaging of silicone gel-filled breast implants in vivo with a method that visualizes silicone selectively. J Magn Reson Imaging. 1993;3(5):713-7. 10.1002/jmri.18800305056.
6. Glynn C, Litherland J. Imaging breast augmentation and reconstruction. Br J Radiol. 2008;81(967):587-95. 10.1259/bjr/615678847.
7. Stelter JKB, C.; Ruschke, S.; Weiss, K.; Diefenbach, M. N.; Wu, M.; Borde, T.; Makowski, M. R.; Fallenberg, E. M.; Karampinos, D. C. Optimal experimental design for quantitative water, fat and silicone separation using a variable projection method with 4 or 6 echoes at 3T. Proc Intl Soc Mag Reson Med. 2021;16, p. 1517, 2021.
8. Ruschke S, Eggers H, Kooijman H, Diefenbach MN, Baum T, Haase A, et al. Correction of phase errors in quantitative water-fat imaging using a monopolar time-interleaved multi-echo gradient echo sequence. Magn Reson Med. 2017;78(3):984-96. 10.1002/mrm.264859.
9. Juanpere S, Perez E, Huc O, Motos N, Pont J, Pedraza S. Imaging of breast implants-a pictorial review. Insights Imaging. 2011;2(6):653-70. 10.1007/s13244-011-0122-3
Figures