0145
High Spatiotemporal Resolution Breast MR Increases Cancer Detection and Reduces Unnecessary Biopsies in Patients with Marked BPE1Memorial Sloan Kettering Cancer Center, New York, NY, United States
Synopsis
Contrast-enhanced breast MRI is a powerful tool for breast cancer detection, but can be limited in the setting of marked background parenchymal enhancement (BPE), which can mask underlying lesions. We found that among patients with marked BPE, positive predictive value (PPV2) and cancer detection rate (CDR) were statistically significantly increased when the high spatial/high temporal resolution protocol, rather than the standard protocol, was used. The interval cancer rate was not significantly different between these groups.
Introduction
Contrast-enhanced breast MRI is the most sensitive tool for cancer detection, outperforming mammography and ultrasound combined.1 Breast cancers enhance on MRI at a very early stage due to tumor angiogenesis, which is present in lesions as small as 2-3mm.2 However, the normal fibroglandular tissue can also enhance, termed background parenchymal enhancement (BPE), which can obscure small underlying cancers (masking effect) and has been associated with higher abnormal interpretation rates.3 Since malignant lesions demonstrate fast initial enhancement whereas benign lesions and BPE have a slower and persistent rate of enhancement, simultaneous high temporal and spatial breast MRI can be used to differentiate these kinetic patterns to further improve diagnostic performance.4,5,6 High resolution breast MRI has demonstrated high diagnostic accuracy, however, the extent to which high temporal and high spatial resolution breast MRI can improve the diagnostic accuracy of breast MRI in patients with marked background parenchymal enhancement has not yet been characterized. The purpose of this abstract is to evaluate whether breast MRI performance metrics for marked BPE exams improve when a simultaneous high temporal and spatial, rather than a standard breast MRI protocol, is used.Materials and Methods
In this IRB-approved HIPPA-compliant retrospective study, consecutive contrast-enhanced breast MRI exams performed at our institution from January 1, 2016-December 31, 2016 and from January 1, 2019-December 31, 2019, were included. All breast MRI exams were performed on a 1.5 or 3.0 Tesla system (Discovery 750, GE Medical Systems, Waukesha, WI) using a dedicated 8- or 16- channel breast coil and a gadolinium-based contrast agent. Exams from 2016 were performed using a standard breast MRI protocol (spatial resolution 1mm isotropic, temporal resolution 90 secs) with 3 post-contrast phases. Exams from 2019 were performed using a simultaneous high temporal and spatial DISCO protocol (temporal resolution 12-16 secs, in-plane 1mm, SI 1-1.3mm). The positive predictive value (PPV2), cancer detection rate (CDR), and interval cancer rate (ICR) were calculated for the 2016 and 2019 groups. Interval cancers were defined as a diagnosis of cancer that occurred less than 365 days following the breast MRI exam. Cases were also subdivided according to BPE category, and the PPV2, CDR and ICR were calculated for these subgroups. The PPV2, CDR and ICR from 2016 and 2019 were compared for the marked BPE subgroup, and for all cases. A two-proportion Z-test was calculated with Bonferroni correction to evaluate for statistical significance (α = 0.025).Results
There were 4,420 breast MRIs performed in 2016 with the standard protocol and 5,550 breast MRIs performed in 2019 with the DISCO protocol. Patient and exam characteristics are shown in Table 1. For the Marked BPE subgroup, PPV2 was higher with the DISCO protocol than with the standard protocol (26/51 (50.1%) v. 8/42 (19.1%), p = 0.00074), the CDR was higher with the DISCO protocol than with the standard protocol (26/315 (8.25%) v. 8/261 (3.10%), p = 0.004), and the interval cancer rate was not significantly different (1/315 (0.32%) v. 1/261 (0.38%, p = 0.896). Across the full dataset (all BPE categories), PPV2, CDR and ICR were not statistically significantly different between 2016 and 2019 (see Table 2 and Figure 1 for details). Figure 2 shows an example of a cancer case with marked BPE that benefited from the DISCO protocol.Discussion
Our results show that for patients with marked BPE, the simultaneous high temporal and spatial MRI protocol results in both more cancers detected and in fewer unnecessary biopsies compared to the standard breast MRI protocol. Such simultaneous high temporal and spatial breast MRI protocols have been implemented at a few major academic medical centers but are not routinely used in smaller centers or private practices. This work suggests patients with marked BPE should be imaged with such a protocol to maximize cancer detection and minimize unwarranted biopsies. Since the high resolution protocol imaging was introduced for some cases at our institution during 2017 but did not become the standard protocol for all cases until towards the end of 2018, we decided to include MRIs from 2016 and 2019 in this initial analysis as a simple way to distinguish the two protocol types, although further work is needed to sort the 2017 and 2018 MRIs by protocol type as a way to expand the size of this analysis.Conclusion
For patients with marked background parenchymal enhancement (BPE), a simultaneous high temporal and spatial breast MRI protocol increases PPV2 and increases CDR. Further evaluation with larger numbers of patients and from multiple institutions is needed to confirm the experience of this single large tertiary care cancer center.Acknowledgements
Thank you to Cathi Johnson for sharing biopsy results data for this project.References
1. Kuhl C, Weigel S, Schrading S, Arand B, Bieling H, König R, et al. Prospective multicenter cohort study to refine management recommendations for women at elevated familial risk of breast cancer: the EVA trial. J Clin Oncol. 2010;28(9):1450-7. Epub 20100222. doi: 10.1200/JCO.2009.23.0839. PubMed PMID: 20177029.
2. Hillen F, Griffioen AW. Tumour vascularization: sprouting angiogenesis and beyond. Cancer Metastasis Rev. 2007;26(3-4):489-502. doi: 10.1007/s10555-007-9094-7. PubMed PMID: 17717633; PubMed Central PMCID: PMC2797856.
3. DeMartini WB, Liu F, Peacock S, Eby PR, Gutierrez RL, Lehman CD. Background parenchymal enhancement on breast MRI: impact on diagnostic performance. AJR Am J Roentgenol. 2012;198(4):W373-80. doi: 10.2214/AJR.10.6272. PubMed PMID: 22451576.
4. Pinker K, Grabner G, Bogner W, Gruber S, Szomolanyi P, Trattnig S, et al. A combined high temporal and high spatial resolution 3 Tesla MR imaging protocol for the assessment of breast lesions: initial results. Invest Radiol. 2009;44(9):553-8. doi: 10.1097/RLI.0b013e3181b4c127. PubMed PMID: 19652611.
5. Mann RM, Mus RD, van Zelst J, Geppert C, Karssemeijer N, Platel B. A novel approach to contrast-enhanced breast magnetic resonance imaging for screening: high-resolution ultrafast dynamic imaging. Invest Radiol. 2014;49(9):579-85. doi: 10.1097/RLI.0000000000000057. PubMed PMID: 24691143.
6. van Zelst JCM, Vreemann S, Witt HJ, Gubern-Merida A, Dorrius MD, Duvivier K, et al. Multireader Study on the Diagnostic Accuracy of Ultrafast Breast Magnetic Resonance Imaging for Breast Cancer Screening. Invest Radiol. 2018;53(10):579-86. doi: 10.1097/RLI.0000000000000494. PubMed PMID: 29944483.
Figures
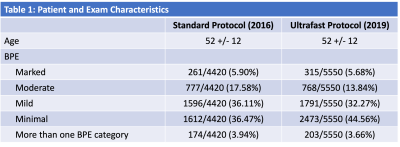
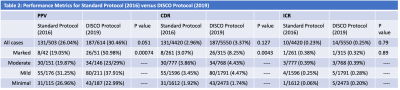
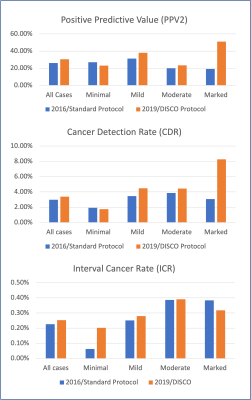
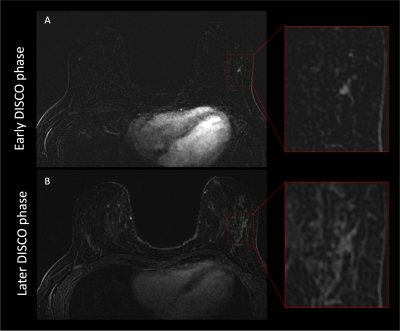
Figure 2. 50 year old women with left axillary metastases of unknown origin. Breast MRI performed to search for the primary tumor. On early DISCO phase (A), a small 0.4 cm irregular mass is identified in the left lateral breast but on later phases (B) the mass is obscured by background parenchymal enhancement, highlighting the importance of high temporal and high spatial resolution.