0098
Improving diagnostic confidence using a Deep-Learning Reconstructed Fast Motion-Robust PROPELLER protocol for Shoulder Imaging
1GE Healthcare, Madrid, Spain, 2Rey Juan Carlos University, Madrid, Spain, 3GE Healthcare, Houston, TX, United States, 4Clínica Cemtro, Madrid, Spain, 5GE Healthcare, Colorado, CO, United States, 6GE Healthcare, New York, NY, United States
Synopsis
PROPELLER imaging is the choice for motion-prone anatomies, to generate good diagnostic quality images even for challenging patients. However, it is associated with prolonged scan times. In this study we evaluate the application of a new DL-based reconstruction algorithm to enhance a fast PROPELLER shoulder protocol with the goal of providing consistent diagnostic confidence and an overall improved image quality compared to conventional routine protocols. Our study demonstrates the proposed under 10min shoulder MRI protocols are interchangeable and have the same diagnostic confidence with better SNR and lesion conspicuity than routine MRI protocols for shoulder post-contrast and instability exams.
Background
Motion is a common cause of artifacts in shoulder MRI that may mask true pathology and make an exam not usable diagnostically. Re-scans and patient call backs are no longer options for managing unexpected results.Periodically Rotated Overlapping ParallEL Lines with Enhanced Reconstruction (PROPELLER)1 is the choice for the imaging of motion-prone anatomies including musculoskeletal (MSK) exams, to generate consistently good, diagnostic quality images even for challenging patients and difficult-to-image anatomies2,3,4. Although PROPELLER can reduce motion, it is often associated with prolonged scan times since the oversampling is not confined to a single axis.
Fortunately, the field of MR research and development is actively exploring alternatives to conventional MR reconstruction to address trade-offs between spatial resolution, signal-to-noise ratio (SNR) and scan time.
The purpose of this study is to evaluate the application of a new deep-learning (DL) reconstruction algorithm5,6 to enhance a fast PROPELLER shoulder protocol. We hypothesized that while providing a beneficial decrease in acquisition time, DL Recon method would provide consistent diagnostic information and an overall improved image quality compared to conventional routine protocols.
Data Acquisition Methods
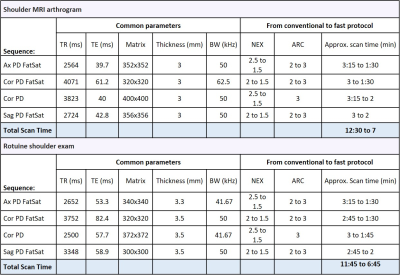
14 patients were recruited in Clinica Cemtro, Madrid (Spain), prior approval from Ethics Committee. 7 patients underwent MRI arthrogram whereas the other 7 patients were referred for a routine exam due to glenohumeral shoulder instability. All MRI examinations were performed on a 3T SIGNA™ Architect (GE Healthcare, Waukesha, WI) scanner using a 20-channel multi-purpose AIRTM coil.For each group of patients, two protocols were scanned, the corresponding conventional clinical protocol and a faster version. Both included four proton density (PD) weighted PROPELLER sequences as shown in table 1. To reduce scan time, number of excitations (NEX) was set to 1.5 and acceleration factor was increased to 3 in all the series whereas the other acquisition parameters were kept the same as in the routine protocols. In the routine protocols, the total scan time of these four sequences is approximately 12min in average, while it is approximately 7min in the fast protocols. The typical parameters used in this study are shown in Table 1.
Images were generated from the Fast PROPELLER protocol raw data with the DL recon method5,6 that uses a deep convolutional residual encoder network trained to reconstruct images with reduction in noise and artifacts (tuned to 75% noise reduction for this work), whereas those from routine protocols were obtained with conventional reconstruction.
Data Analysis Methods
To quantify image quality improvement from an objective perspective, apparent SNR was measured as the mean signal value divided by the standard deviation (SD) on a region of interest (ROI) placed at a uniform muscle location next to the chest. The ROI was placed at the same location in Coronal PD FatSat and Coronal PD sequences from both routine and fast protocols for each patient.To validate clinical utility, two radiologists with 20 and 5 years of experience in MSK imaging independently reviewed the proposed fast protocol against the conventional one rating the equivalence (worse, equivalent, better) in terms of SNR, sharpness, overall image quality (IQ) and lesion conspicuity. Feedback on diagnostic confidence and any other issue were also captured.
A paired ratio t-test was used to compare SNR between both protocols (GraphPad Prism version 7, California, USA) and inter-rater agreement was assessed using Cohen’s kappa (K) (SPSS software package version 22; IBM, Armonk, NY).
Results
Scan time was reduced in 40% in average for all the patients, resulting in fast exams under 10min. This significant time saving has the potential to improve patient workflow as well as increase patient comfort and reduce probability of motion artifacts.In this work, the ratio (SNRFast+DL/SNRroutine) was used to quantify the effect of the DL recon algorithm to avoid subject and scan variance.
Paired ratio t-tests showed DL recon applied on the fast exam significantly improved the SNR for both sequences assessed (p < 0.0001). According to the mean of the ratios (SNRFast+DL/SNRroutine), SNR values computed on fast DL recon images are about double the routine values (Figure 1).
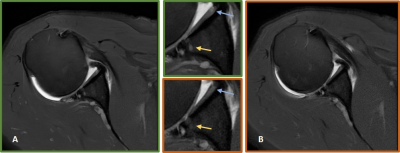
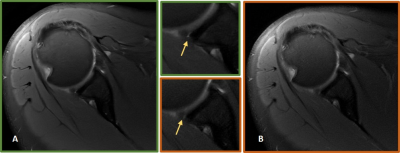
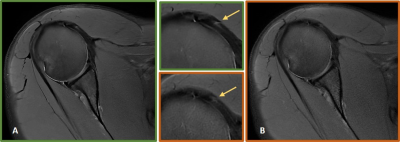
Regarding the clinical assessment, both readers completely agreed on grading DL Recon images as better than routine ones in terms of SNR, sharpness and overall IQ for 100% of the cases. Regarding lesion conspicuity, the more experienced radiologist classified DL fast protocol as better than routine in more cases than the other reader - in 79% versus 57% of all the cases, being the remaining ones classified as equivalent. This leads to a Kappa score of 0.533 (p<0.5) and a raw agreement of 71,5%. The experienced reader found a few small lesions better depicted on DL images providing a higher diagnostic confidence. These findings did not change the overall diagnosis but would have added more value to it (Figures 2, 3, 4).
Conclusion
When enhanced by a deep learning reconstruction algorithm, PROPELLER sequence is promising to facilitate substantial time savings without compromising interobserver agreement for evaluation of clinically relevant pathology, and even providing superior overall IQ and better lesion conspicuity compared to routine protocol.Our study demonstrates the proposed fast under 10min shoulder MRI protocol is interchangeable and has the same diagnostic confidence than routine MRI protocol for shoulder post-contrast and shoulder instability exams.
Acknowledgements
No acknowledgement found.References
1. Pipe JG. Motion correction with PROPELLER MRI: application to head motion and free-breathing cardiac imaging. Magn Reson Med 1999; 42:963-969.
2. Fellner C, Menzel C, Fellner F, et al. BLADE in sagittal T2-weighted MR imaging of the cervical spine. AJNR 2010; 31:674–681
3. Hirokawa Y, Isoda H, Maetani Y, Arizono S, Shimada K, Togashi K. Evaluation of motion correction effect and image quality with the periodically rotated overlapping parallel lines with enhanced reconstruction (PROPELLER) (BLADE) and parallel imaging acquisition technique in the upper abdomen. J Magn Reson Imaging 2008; 28: 957–962
4. Dietrich, T., Ulbrich, E., Zanetti, M., Fucentese, S. and Pfirrmann, C. PROPELLER Technique to Improve Image Quality of MRI of the Shoulder. American Journal of Roentgenology 2011; 197(6):1093-1100.
5. Lebel R. Performance characterization of a novel deep learning-based MR image reconstruction pipeline. https://arxiv.org/abs/2008.06559. Published 2020. Accessed Nov 2021.
6. Xinzeng Wang, Daniel Litwiller, Marc Lebel, Ali Ersoz, Lloyd Estkowski, Jason Stafford, Ersin Bayram. High resolution T2W imaging using deep learning reconstruction and reduced field-of-view PROPELLER, ISMRM 2020: 820
Figures