0093
Evaluation inflammatory and chronic structural sacroiliac joint changes in Axial Spondyloarthritis using semiquantitative MRI scoring system1First Central Clinical College, Tianjin Medical University, Tianjin, Tianjin, China, 2Tianjin First Central Hospital, Tianjin, Tianjin, China
Synopsis
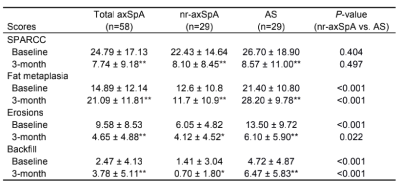
There are many clinical studies investigating the differences between non-radiographic axial spondyloarthritis and ankylosing spondylitis(AS), but few focus on radiology. Spondyloarthritis Research Consortium of Canada (SPARCC) and Sacroiliac Joint Structural Score (SSS) scoring systems can assess a broad spectrum of inflammatory and structural lesions. Our results indicate SPARCC scores were significantly improved after treatment. A significant increase in SSS scores for fat metaplasia and backfill was noted. Therefore, using semiquantitative MRI scoring methods can assess abnormal lesions and treatment response. Higher structural damages were seen in AS patients. SPARCC can assess severity of disease pre-treatment and treatment effectiveness.
Introduction
Axial spondyloarthritis (axSpA) is a chronic, inflammatory rheumatic disease. Patients with axSpA can be grouped into non-radiographic axial spondyloarthritis (nr-axSpA) and AS [1]. There are many clinical studies investigating the differences, but few focus on radiology. Magnetic resonance imaging (MRI) is established as the imaging arm for diagnosing and managing axSpA [2]. Systematic MRI scoring systems of sacroiliac joint(SIJ) have been developed and validated. However, there has been limited assessment in clinical trials, and little is known regarding the impact of therapy. In this study, we assess the inflammatory and structural MRI findings in axSpA patients and to investigate the treatment effectiveness with tumor necrosis factor-alpha (TNFα) inhibitor using MRI-based scoring systems.Methods
This study was a retrospective longitudinal cohort study. Patients were diagnosed as axSpA according to the 2009 Assessment of SpondyloArthritis international Society (ASAS) criteria (AS had radiographic sacroiliitis meeting the Modified New York Criteria) [2]. Baseline and 3-month MRIs were available for 58 patients with axSpA. These patients are the first visit and have sacroiliitis at baseline.Sequences and parameters: All patients were scanned using a 3.0 T MR scanner (Ingenia, Philips Healthcare, the Netherlands). All sequences were obtained by scanning in the oblique coronal plane parallel to the sacrum plane. The scanning sequences and parameters were as follows: T1-weighted images (T1WI) mDixon-TSE (TR, 550 ms; TE, 16 ms; FOV, 220 × 220 mm; slice thickness, 3 mm; slice gap, 0 mm; matrix, 276 × 210), T2-weighted images (T2WI) mDixon-TSE (TR, 2300 ms; TE, 90 ms; FOV, 220 × 220 mm; slice thickness, 3 mm; slice gap, 0 mm; matrix, 276 × 219).
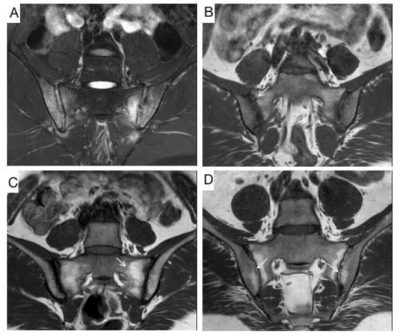
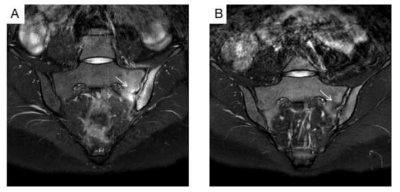
Image evaluation: All MRIs were evaluated for bone marrow edema(BME) according to SPARCC method [3]. To evaluate inflammation, dividing the bilateral joint into four quadrants, scored dichotomously. An additional score was given when both sides of the joint with a BME signal of depth ≥ 1 cm or an intense signal, respectively. All MRIs were evaluated for chronic findings according to SPARCC SSS method. The system was used to assess the structural lesions on T1WI [4]. The presence/absence of lesions is scored in SIJ quadrants (fat metaplasia, erosion) or halves (backfill, ankylosis).
Statistical analysis: All data were statistically analysed using SPSS 26.0 software. Demographic, clinical, and MRI data were described in terms of percentages and numbers (qualitative) or means and standard deviations (SD) (quantitative). Analyses were performed using the mean scores of the two readers. Statistical analyses included chi-square tests, independent t-tests, and paired t-tests. Associations between changes in parameters of inflammation (C-reactive protein, Erythrocyte Sedimentation Rate, SPARCC score), SSS subgroups scores were examined by correlation analyses using Spearman correlation analysis. Interobserver reliability for scores was assessed using the intraclass correlation coefficient (ICC). Values of P<0.05 were considered statistically significant.
Results
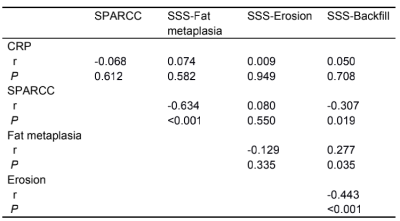
At baseline,the mean ± SD SPARCC score was 24.79 ± 17.13 and SSS score was 36.47 ± 24.15. Higher SPARCC score was seen in AS group, however, there was no significant difference. In SSS scores, significant differences were found between AS and nr-axSpA groups in fat metaplasia, erosion, and backfill(Table 1,Figure 3). After treatment, SPARCC scores were significantly improved in both groups (P<0.001). However, there were no statistically significant difference between both groups. As for SSS scores, a significant increase in SSS scores for fat metaplasia and backfill (P< 0.001, P<0.001, respectively) and decrease in SSS score for erosion (P<0.05) was noted in both groups (Table 1,Figure 3). Change in SPARCC score correlated inversely with changes in SSS scores for fat metaplasia (r=-0.634, P<0.001) and backfill (r=-0.307, P<0.05). Change in SSS score for backfill correlated positively with the change in fat metaplasia (r = 0.277, P<0.05) and inversely with the change in backfill (r=-0.443, P<0.001) (Table 2).Discussion
At baseline, we observed the distribution pattern of structural lesions may differ between AS and nr-axSpA patients; fat metaplasia is seen more in AS patients. Almost all AS patients have bilateral fat metaplasia and erosion. Therefore, we believe that nr-axSpA may occur in the early stage, and may be less severe.In this study, SPARCC scoring system provides a reference for evaluating treatment efficacy. We observed that anti-TNFα therapy have significant efficacy. Furthermore, we found that there were significant changes of fat metaplasia and backfill. Our results are consistent with those of a previous study that fat metaplasia and backfill are early post-inflammatory changes which most likely reflect the early stages of bone remodelling [5-7]. The histological is not clear. The disturbance of the homeostasis between osteoblasts and osteoclasts may be a crucial reason for new bone formation [8].Conclusion
In conclusion, using the semiquantitative MRI-based scoring methods can assess inflammatory and structural lesions and the treatment response in the axSpA. Higher structural damages were seen in AS patients. SPARCC can be used to assess disease severity and assess treatment effectiveness.Acknowledgements
No acknowledgement found.References
1. Sieper J, Braun J, Dougados M, Baeten D: Axial spondyloarthritis. Nat Rev Dis Primers 2015, 1:15013.
2. Sieper J, Rudwaleit M, Baraliakos X, Brandt J, Braun J, Burgos-Vargas R, Dougados M, Hermann KG, Landewe R, Maksymowych W et al: The Assessment of SpondyloArthritis international Society (ASAS) handbook: a guide to assess spondyloarthritis. Ann Rheum Dis 2009, 68 Suppl 2:ii1-44.
3. Maksymowych WP, Inman RD, Salonen D, Dhillon SS, Williams M, Stone M, Conner-Spady B, Palsat J, Lambert RG: Spondyloarthritis research Consortium of Canada magnetic resonance imaging index for assessment of sacroiliac joint inflammation in ankylosing spondylitis. Arthritis Rheum 2005, 53(5):703-709.
4. Maksymowych WP, Wichuk S, Chiowchanwisawakit P, Lambert RG, Pedersen SJ: Development and preliminary validation of the spondyloarthritis research consortium of Canada magnetic resonance imaging sacroiliac joint structural score. J Rheumatol 2015, 42(1):79-86.
5. Maksymowych WP, Wichuk S, Chiowchanwisawakit P, Lambert RG, Pedersen SJ: Fat metaplasia and backfill are key intermediaries in the development of sacroiliac joint ankylosis in patients with ankylosing spondylitis. Arthritis Rheumatol 2014, 66(11):2958-2967.
6. Song IH, Hermann KG, Haibel H, Althoff CE, Poddubnyy D, Listing J, Weiss A, Freundlich B, Rudwaleit M, Sieper J: Relationship between active inflammatory lesions in the spine and sacroiliac joints and new development of chronic lesions on whole-body MRI in early axial spondyloarthritis: results of the ESTHER trial at week 48. Ann Rheum Dis 2011, 70(7):1257-1263.
7. Chiowchanwisawakit P, Lambert RG, Conner-Spady B, Maksymowych WP: Focal fat lesions at vertebral corners on magnetic resonance imaging predict the development of new syndesmophytes in ankylosing spondylitis. Arthritis Rheum 2011, 63(8):2215-2225.
8. Baraliakos X, Boehm H, Bahrami R, Samir A, Schett G, Luber M, Ramming A, Braun J: What constitutes the fat signal detected by MRI in the spine of patients with ankylosing spondylitis? A prospective study based on biopsies obtained during planned spinal osteotomy to correct hyperkyphosis or spinal stenosis. Ann Rheum Dis 2019, 78(9):1220-1225.
Figures