0090
Efficient 3D dark-blood thoracic and abdominal aortic imaging with novel motion-corrected water/fat DANTE sequence1School of Biomedical Engineering and Imaging Sciences, King's College London, London, United Kingdom, 2MR Research Collaborations, Siemens Healthcare Limited, Frimley, United Kingdom
Synopsis
Dark-blood imaging is a promising tool for vessel wall assessment in cardiovascular disease. Here we introduce a novel water/fat DANTE-prepared sequence for 3D dark-blood imaging of the thoracic and abdominal aorta. The sequence integrates image navigation to enable respiratory motion correction resulting in a predictable scan time. Results from healthy subjects show the feasibility of the sequence for depicting the aortic wall with high-resolution with an overall short scan of ~6 minutes.
Introduction
Dark-blood cardiovascular MR imaging techniques provide an excellent tool for the assessment of plaque burden in atherosclerosis and detection of thrombosis, for instance in patients with abdominal aortic aneurysms. Conventional dark-blood techniques rely on through-plane blood flow to null the blood signal and therefore are limited to 2D acquisitions, limiting their application for imaging the thoracic and abdominal aorta. More recently, 3D imaging techniques which use preparation pulses and/or variable flip angle readouts have been introduced to enable dark-blood imaging with higher spatial resolution and improved spatial coverage. These techniques include variable-flip-angle turbo spin echo1, motion-sensitized driven equilibrium2, and delay alternating with nutation for tailored excitation (DANTE)3,4.While these techniques have shown promising results for the depiction of the aortic vessel wall, some challenges remain for wider use in clinical practice. Firstly, to minimize the effect of respiratory motion, they either use averaging resulting in blurred images, or diaphragmatic navigator gating which leads to longer and unpredictable scan times. Furthermore, when imaging the thoracic and abdominal aorta, a robust mechanism that can suppress fat signal in a large field of view is required.
In this study we introduce a novel sequence for dark-blood imaging of the thoracic and abdominal aorta, which uses a DANTE preparation pulse to achieve blood signal suppression, a dual-echo Dixon gradient-echo readout for robust fat suppression and integrates an image navigator (iNAV) for respiratory motion correction to enable a short and predictable scan of ~6 minutes.
Methods
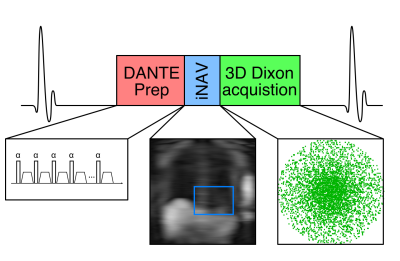
Image acquisition consists of an ECG-triggered dual-echo 3D DANTE-prepared spoiled gradient echo prototype sequence (Fig 1). 3D dual-echo data are acquired with an undersampled variable-density golden-step Cartesian trajectory with spiral profile order sampling5. The image reconstruction pipeline has been described in detail elsewhere6. In brief, coronal dual-echo 2D iNAVs are acquired using low flip-angle excitation pulses before the 3D acquisition and are used to estimate superior-inferior (SI) and right-left (RL) motion by tracking a template around the heart. The estimated SI motion is used to sort the 3D dual-echo data into equally populated bins, and 3D MR images reconstructed at each respiratory position are used to estimate non-rigid motion between bins. 2D translational beat-to-beat and 3D non-rigid bin-to-bin motion is then integrated into a motion-compensated reconstruction with patch-based low-rank regularization to produce motion-compensated dual echo images, which are used to compute the final 3D water/fat DANTE images.Nine healthy subjects (4 male, age 31±2 years old) were scanned on a 1.5T system (MAGNETOM Aera, Siemens Healthcare, Erlangen, Germany) with the proposed water/fat DANTE sequence. Data were acquired with the following parameters: coronal orientation, 1.4mm3 isotropic resolution, field of view=400x300x100-125mm3, flip angle=15°, TE1/TE2/TR=2.38/4.76/6.83ms, bandwidth=495Hz/px, subject-specific mid-diastolic acquisition window (110-150ms), 3-fold undersampling. The DANTE preparation pulse used a flip angle =15° and pulse train length =150.
Results
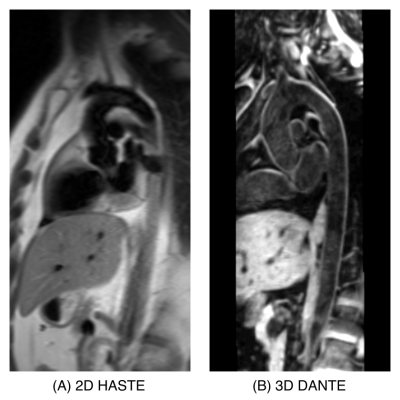
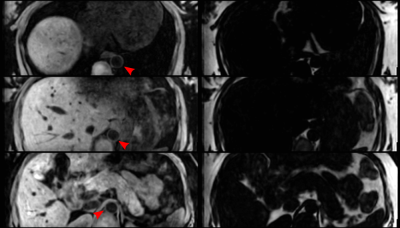
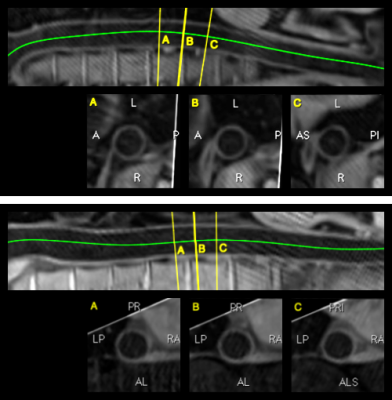
Scans were completed in all subjects with a mean±SD scan time of 5.6±0.7 min. Fig 2 shows an example of a reformatted long axis view of the aorta, alongside a conventional 2D HASTE dark-blood image for a representative subject. A good depiction of the aortic wall can be observed in the 3D DANTE image, which has higher resolution, increased volumetric coverage, and excellent fat suppression throughout the field of view. This can be further observed in Fig 3, where transverse slices of the water/fat DANTE images can be observed at different levels of the aorta for an additional subject. A curved reformatting from two further subjects can be seen in Fig 4, alongside transverse views at three locations, showing the potential for the proposed sequence to enable vessel wall imaging of the thoracic and abdominal aorta from a short efficient scan.Conclusion
We have demonstrated the feasibility of a novel dark-blood DANTE-prepared water/fat sequence for imaging the thoracic and abdominal aorta. Future work includes validation of the sequence in patients with aortic pathologies.Acknowledgements
This work was supported by the following grants: (1) EPSRC EP/P032311/1, EP/P007619/1, EP/P001009/1; (2) BHF programme grant RG/20/1/34802 and (3) Wellcome/EPSRC Centre for Medical Engineering (WT 203148/Z/16/Z).References
1. Mihai G, Chung YC, Merchant A, Simonetti OP, Rajagopalan S. T1-weighted-space dark blood whole body magnetic resonance angiography (DB-WBMRA): Initial experience. J Magn Reson Imaging 2010;31:502–9.
2. Koktzoglou I, Li D. Diffusion-prepared segmented steady-state free precession: Application to 3D black-blood cardiovascular magnetic resonance of the thoracic aorta and carotid artery walls. J Cardiovasc Magn Reson 2007;9:33–42.
3. Li L, Miller KL, Jezzard P. DANTE-prepared pulse trains: A novel approach to motion-sensitized and motion-suppressed quantitative magnetic resonance imaging. Magn Reson Med 2012;68:1423–38.
4. Zhu C, Haraldsson H, Faraji F, Owens C, Gasper W, Ahn S, et al. Isotropic 3D black blood MRI of abdominal aortic aneurysm wall and intraluminal thrombus. Magn Reson Imaging 2016;34:18–25.
5. Prieto C, Doneva M, Usman M, Henningsson M, Greil G, Schaeffter T, et al. Highly efficient respiratory motion compensated free-breathing coronary MRA using golden-step Cartesian acquisition. J Magn Reson Imaging 2015;41:738–46.
6. Munoz C, Bustin A, Neji R, Kunze KP, Forman C, Schmidt M, et al. Motion-corrected 3D whole-heart water-fat high-resolution late gadolinium enhancement cardiovascular magnetic resonance imaging. J Cardiovasc Magn Reson 2020;22:53.
Figures