0024
Free-Breathing Cardiac Cine MRI with Compressed Sensing Real-Time Imaging and Respiratory Motion Correction: Initial Pediatric Experience1Siemens Medical Solutions USA Inc., Chicago, IL, United States, 2Siemens Medical Solutions USA Inc., Houston, TX, United States, 3Siemens Medical Solutions USA Inc., Los Angeles, CA, United States, 4Siemens Healthcare, Erlangen, Germany, 5Texas Children's Hospital, Houston, TX, United States
Synopsis
Cardiac cine MRI plays an important role in evaluating cardiac function. The conventional technique, 2D segmented acquisition with retrospective electrocardiogram gating, requires breath-holding and therefore is challenging for many types of patients such as young children. In this work, we report our initial experience of a recently developed free-breathing cardiac cine MRI technique on pediatric patients undergoing routine CMR. Our results showed that the proposed technique, based on compressed sensing real-time imaging and respiratory motion correction, produced comparable quantitative LV measurements and image quality to the reference breath-hold technique in a wide range of patient sizes and ages.
Introduction
Cine MRI is an important diagnostic tool for evaluating cardiac function (1, 2) and an essential component of most cardiac magnetic resonance (CMR) protocols (3). The current standard technique, 2D segmented acquisition with retrospective electrocardiogram (ECG) gating (4), requires repeated breath-holding (5) that can be challenging for many patients. On young children, reliable breath-holding may only be achieved under general anesthesia with mechanical ventilation, which adds to the cost, risk, and complexity of CMR (6). Furthermore, breath-holding complicates the exam workflow due to the necessary patient recovery time. The operator must also check the image quality and reattempt the scan when the images are corrupted by respiratory motion. Therefore, free-breathing cine MRI is desirable for improving patient experience, simplifying workflow, and achieving robust image quality in wider patient population. Recently, we proposed a prototype free-breathing cardiac cine imaging technique, real-time compressed sensing cine with motion correction (RTCSCineMoCo) (7). This technique combines highly accelerated real-time acquisition, compressed sensing (CS) reconstruction, and retrospective, fully automated respiratory motion correction. In this work, we report our initial clinical experience of RTCSCineMoCo on pediatric patients undergoing routine CMR exams at a single center. We compare it with the standard breath-hold cardiac cine technique in terms of quantitative cardiac function measurements and subjective image quality scores.Methods
With institutional IRB approval and written consent form, we acquire both breath-hold segmented cine with retrospective ECG gating (BH) and free-breathing RTCSCineMoCo images on 15 patients using a clinical 1.5T MR scanner (MAGNETOM Aera, Siemens Healthcare, Erlangen, Germany). The patient demographic data are as follows: 7.3 ± 5.4 years, range 11 weeks - 19 years; weight 29.7 ± 25.6 kg, range 3.5 – 106.0 kg; 12 males. The sequence parameters were as follows: 11-14 short axis slices, balanced steady-state free precession readout, flip angle = 58-90°, 25 calculated cardiac phases, in-plane resolution = 1.2-1.8 mm for BH, 1.4-2.0 mm interpolated to 0.7-1.0 mm for RTCSCineMoCo, slice thickness = 5.0-9.0 mm; GRAPPA factor = 2 for BH; CS acceleration factor = 9.6-19.2 for RTCSCineMoCo. One reader (MP) manually traced the left ventricle (LV) endocardial contours (QMASS 8.1, Medis Medical System, Leiden, Netherlands), which served as the basis for calculating quantitative LV parameters including end-diastolic volume (EDV), end-systolic volume (ESV), stroke volume (SV), ejection fraction (EF), and cardiac output (CO). In addition, one radiologist experienced in diagnostic CMR (PM, 15 years), blinded to the underlying technique, independently reviewed images from all subjects and scored image quality using a three-point Likert scale (1 = poor image quality and non-diagnostic, 2 = suboptimal image quality but diagnostic, 3 = excellent image quality) in the following categories: (a) myocardial-blood pool contrast, (b) papillary muscle visualization, (c) atrioventricular valve leaflet visualization, (d) wall motion visualization, and (e) visualization of spin dephasing from turbulent flow. We use paired two-tailed t-test to compare the quantitative LV parameters and table time (R 3.5.2, R Core Team, www.R-project.org). We define P=0.05 as statistically significant.Results
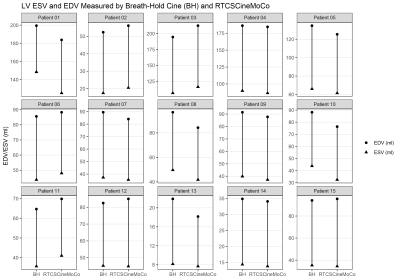
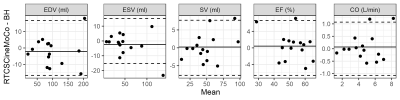
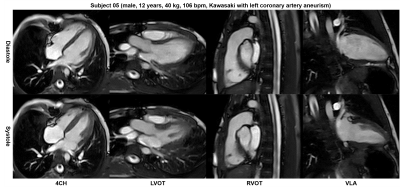
All patients successfully completed the study without complications. The heart rates during cine exams were 98.9 ± 15.4 beats per minute (BPM) for BH and 100.8 ± 14.7 BPM for RTCSCineMoCo (P = 0.47). We found no significant difference between the measured LV function parameters, including EDV (101.1 ± 53.1 ml for BH and 99.0 ± 53.5 ml for RTCSCineMoCo, P = 0.32), ESV (52.1 ± 36.1 ml for BH, 49.8 ± 33.3 ml for RTCSCineMoCo, P = 0.27), SV (49.0 ± 21.8 ml for BH and 49.3 ± 23.4 ml for RTCSCineMoCo, P = 0.82), EF (51.8 ± 9.7% for BH and 52.2 ± 8.5% for RTCSCineMoCo, P = 0.63), and CO (4.7 ± 1.7 L/min for BH and 4.7 ± 1.9 L/min for RTCSCineMoCo, P = 0.62). The two techniques scored identically (3 out of 3) for all five subjective criteria. Fig. 1 and Fig. 2 show the LV EDV and ESV for all patients, and the Bland-Altman plots of the LV function measures, respectively. Fig. 3 shows example images of both diastole and systole phases at mid-ventricular slice positions from four patients, with ages ranging from 11 weeks to 12 years. Fig. 4 shows additional cardiac views obtained with RTCSCineMoCo in one patient.Discussion
In this work, we reported our initial clinical experience of a recently developed free-breathing cardiac cine technique, RTCSCineMoCo, on pediatric subjects from 11 weeks to 19 years undergoing routine CMR exam. The LV function parameters measured from RTCSCineMoCo, including EDV, ESV, SV, EF, and CO, showed no significant difference versus those derived from the conventional breath-hold technique. Both techniques obtained the highest image quality score in all subjective criteria on all subjects. RTCSCineMoCo eliminates the need for manually performed breath-holds for patients under general anesthesia, and may also reduce the need for mechanical ventilation in favor of spontaneous breathing under moderate sedation or while fully conscious (8), thereby lowering the complexity, risk, and resource requirement of pediatric CMR (9-15).Conclusion
In conclusion, we showed that a novel free-breathing cine technique, RTCSCineMoCo, can be implemented in a clinical setting and produce comparable quantitative LV measurements and image quality to the reference breath-hold segmented cine technique.Acknowledgements
No acknowledgement found.References
1. Grothues F, Smith GC, Moon JC, Bellenger NG, Collins P, Klein HU, et al. Comparison of interstudy reproducibility of cardiovascular magnetic resonance with two-dimensional echocardiography in normal subjects and in patients with heart failure or left ventricular hypertrophy. Am J Cardiol. 2002;90(1):29-34.
2. Grothues F, Moon JC, Bellenger NG, Smith GS, Klein HU, Pennell DJ. Interstudy reproducibility of right ventricular volumes, function, and mass with cardiovascular magnetic resonance. Am Heart J. 2004;147(2):218-23.
3. Global Cardiovascular Magnetic Resonance Registry I, Kwong RY, Petersen SE, Schulz-Menger J, Arai AE, Bingham SE, et al. The global cardiovascular magnetic resonance registry (GCMR) of the society for cardiovascular magnetic resonance (SCMR): its goals, rationale, data infrastructure, and current developments. J Cardiovasc Magn Reson. 2017;19(1):23.
4. Carr JC, Simonetti O, Bundy J, Li D, Pereles S, Finn JP. Cine MR angiography of the heart with segmented true fast imaging with steady-state precession. Radiology. 2001;219(3):828-34.
5. Kramer CM, Barkhausen J, Bucciarelli-Ducci C, Flamm SD, Kim RJ, Nagel E. Standardized cardiovascular magnetic resonance imaging (CMR) protocols: 2020 update. J Cardiovasc Magn Reson. 2020;22(1):17.
6. Fratz S, Chung T, Greil GF, Samyn MM, Taylor AM, Valsangiacomo Buechel ER, et al. Guidelines and protocols for cardiovascular magnetic resonance in children and adults with congenital heart disease: SCMR expert consensus group on congenital heart disease. J Cardiovasc Magn Reson. 2013;15:51.
7. Pang J, Leon PI, Bi X, McNeal G, Forman C, Leidecker C, et al. Free-Breathing Cardiac Cine MRI with Compressed Sensing Real-Time Imaging and Retrospective Motion Correction. Annual Meeting International Society for Magnetic Resonance in Medicine; Virtual 2020. p. 2190.
8. Christopher AB, Quinn RE, Zoulfagharian S, Matisoff AJ, Cross RR, Xue H, et al. Motion-corrected cardiac MRI is associated with decreased anesthesia exposure in children. Pediatr Radiol. 2020;50(12):1709-16. 9. Malviya S, Voepel-Lewis T, Eldevik OP, Rockwell DT, Wong JH, Tait AR. Sedation and general anaesthesia in children undergoing MRI and CT: adverse events and outcomes. Br J Anaesth. 2000;84(6):743-8.
10. Morray JP, Geiduschek JM, Ramamoorthy C, Haberkern CM, Hackel A, Caplan RA, et al. Anesthesia-related cardiac arrest in children: initial findings of the Pediatric Perioperative Cardiac Arrest (POCA) Registry. Anesthesiology. 2000;93(1):6-14.
11. Serafini G, Zadra N. Anaesthesia for MRI in the paediatric patient. Curr Opin Anaesthesiol. 2008;21(4):499-503.
12. Kalkman CJ, Peelen L, Moons KG, Veenhuizen M, Bruens M, Sinnema G, et al. Behavior and development in children and age at the time of first anesthetic exposure. Anesthesiology. 2009;110(4):805-12.
13. Ramamoorthy C, Haberkern CM, Bhananker SM, Domino KB, Posner KL, Campos JS, et al. Anesthesia-related cardiac arrest in children with heart disease: data from the Pediatric Perioperative Cardiac Arrest (POCA) registry. Anesth Analg. 2010;110(5):1376-82.
14. Vanderby SA, Babyn PS, Carter MW, Jewell SM, McKeever PD. Effect of anesthesia and sedation on pediatric MR imaging patient flow. Radiology. 2010;256(1):229-37.
15. Schiller RM, Allegaert K, Hunfeld M, van den Bosch GE, van den Anker J, Tibboel D. Analgesics and Sedatives in Critically Ill Newborns and Infants: The Impact on Long-Term Neurodevelopment. J Clin Pharmacol. 2018;58 Suppl 10:S140-S50.
Figures