S92
7T Knee MRI: Clinical Benefits and Challenges
Kevin Epperson1, Karla Epperson1, Garry Gold2, and Feliks Kogan3
1Radiology School of Medicine, Stanford University, Stanford, CA, United States, 2Radiology, Stanford Univeristy, Stanford, CA, United States, 3Radiology - SOM, Stanford Univeristy, Stanford, CA, United States
1Radiology School of Medicine, Stanford University, Stanford, CA, United States, 2Radiology, Stanford Univeristy, Stanford, CA, United States, 3Radiology - SOM, Stanford Univeristy, Stanford, CA, United States
Synopsis
Diagnostic MRI scanning of the knee at 3T offers multiple contrasts and definition of anatomical structures, presenting pathology, and allows quantitative performance methods. MRI scanning at 7T of the knee presents challenges, however the ultra high field system offers improved resolution and SNR for visualization of small morphological changes and translation of quantitative methods when these challenges are satisfied.
Purpose
Knee injuries, chronic knee pain, and invading osteoarthritis (OA) are increasing in occurance1-4, resulting in over 2 million MRI exams performed in the United States each year. Diagnostic MRI scanning at 1.5T and 3.0T is able to visualize anatomical injury and pathology of the knee and offers excellent depiction of soft tissues with multiple contrasts as well as advanced quantitative methods to probe tissue microstructure4-8, however limited SNR makes high-resolution scanning of small morphological changes challenging9. Scanning the knee at 7T MRI systems offer improved resolution for detection of structural changes and translational of quantitative methods to detect the earliest biochemical changes in OA. Although protocol development and applications have been limited at 7T due to lack of access of high field MRI as well as limited clinical potential, revived interest has come from a new clinical approval by the US FDA and European CE for 7T knee imaging opening up the translational potential of these systems. In this work we assess the potential clinical benefits of knee imaging at 7T as well as challenges for imaging at ultra-high magnetic fields. In this work we assess the potential clinical benefits of knee imaging at 7T as well as challenges for imaging at ultra-high magnetic fields.Methods
MRI exams were performed 6 healthy volunteers after informed consent on a 3T whole body scanner (Signa PREMIER XT,GE Healthcare, Waukesha, WI, USA.) with a 16-channel phased array flexible knee coil (Neocoil, Pewaukee, WI, USA) and 7T whole body scanner (7T Magnex, GE Healthcare) with a 28-channel transmit-receive knee coil. The imaging protocol is listed in table 1. In short, we aimed to utilize the increased SNR at 7T to push the resolution of both conventional 2D FSE sequences as well as the new 3D sequences that promise to speed up knee scanning by offering high-resolution images capable of reformatting into any scan plan.MRI scanning at 7T presents challenges and one of the biggest is the increased transmit field (B1) inhomogeneity. Similarly, this also presents a challenge in determining the correct system transmit gain (TG) to ensure that signal (flip angles) in the tissues of interest are optimized. To better determine the optimal transmit gain and minimize shading in tissues of interest, we created a sequence consisting of a 90 degree pulse followed by a crusher gradient to store the magnetization longitudinally and then a fast GRE readout. When the transmit gain of any given region is optimized, this sequence will result in no signal in that area. Thus, this sequence allows us to quickly scan a range of different TGs to determine the optimal TG that minimizes signal in our regions of interest. To compare the benefits of optimizing TG at 7T, we ran the 3D-CUBE sequence once with the system auto-prescan and then again after determining the optimal TG.Results
Potential benefits of 7T MRI knee scanning over 3T are shown in Figure 1. In particular, areas of shortened T2 relaxation times such as tibial cartilage and the deep layers of patellar cartilage are visualized considerably better at 7T. Further, coronal and axial reformats of high-resolution 3D-FSE-CUBE scans show considerably less blurring at 7T compared to 3T. High-resolution and high SNR images can provide MSK Radiologists with important benefits including the ability to reformat images into any oblique scan plane to best visualize and characterize anatomy and pathology. This is illustrated in figure 2 where oblique reformatting is able to demonstrate clearly that a meniscal tear radiates all the way through the meniscus and would require surgical repair while at 3T it is unclear. We also observed the challenges that make robust 7T imaging difficult. Figure 3 shows our manual calibration method for determining the optimal TG. The lack of signal means that TG will optimize the signal in that area while high tissue signal means poor TG for that particular area. Scanning at 3T, this is not a problem as the B1 field is fairly uniform and the MR system does a good job of correctly identifying the correct TG. However, at 7T we routinely see that the MR system determines a TG that is 10-15 decibels off of the optimal TG for the areas we are interested in clinically such as the patella-femoral and the tibio-femoral joints. This type of determined TG will cause in a 20-30% error in flip angle resulting in signal loss, blurring, and potentially even lost visualization of pathology (Figure 4). It is critical to develop methodology and training to ensure that 7T images can be correctly and robustly acquired prior to translation into clinical practice.Conclusion
Knee MRI scanning at 3T offers diagnostic quality images with multiple contrasts in soft tissue and visualization of anatomy and pathology. Ultra-high field MR scanning at 7T provides increased resolution and SNR to image microstructures and morphological changes in soft tissue anatomy. Challenges in 7T will require solutions for optimal imaging such as the inhomogeneity of the B1 field. Using optimized TG to correct for shading and ensure flip angles of the tissue of interest provided the correction needed to overcome one such challenge.Acknowledgements
No acknowledgement found.References
Figures
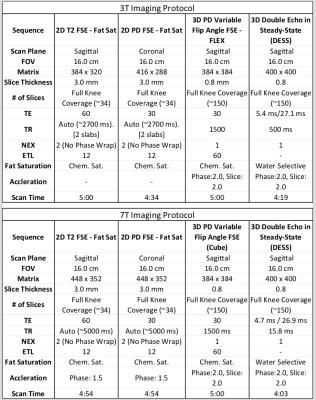
Table 1. Imaging Parameters
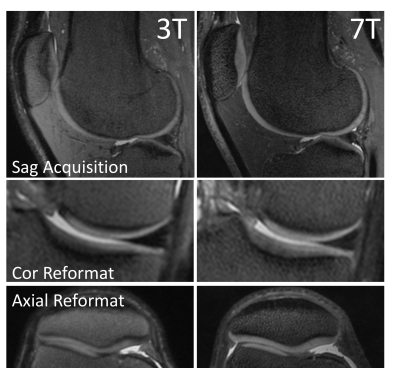
Figure 2. 3D PD Cones images acquired at 3T (left) and 7T (right) with equivalent parameters. 7T images shown considerably better tissue signal and contrast in the deep layers of patellar and tibial cartilage. Additionally, on coronal and axial reformats, 7T images show improved visualization of structures with reduced blurring.
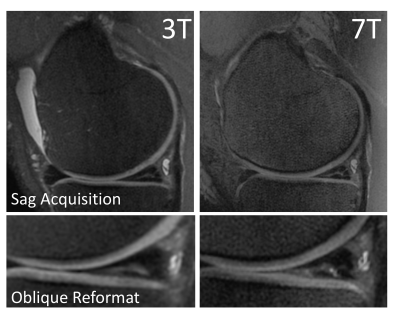
Figure 3: 3D PD Cones images acquired at 3T (left) and 7T (right) both show a meniscal tear in the posterior horn of the medial meniscus. However, oblique reformatting is able to clearly demonstrate that a meniscal tear radiates all the way through the meniscus and would require surgery while this is unclear at 3T.
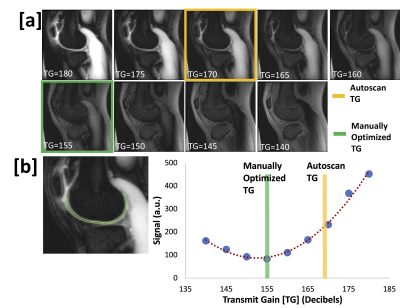
Figure 4: [a] Images from the manual calibration method for determining the optimal TG. A lack of signal represents areas with optimized TG while high tissue signal means a poor TG for that area. [b] By assessing signal in a the areas of interest (cartilage, meniscus, etc) we can determine which TG minimizes signal and utilize that TG for our scan protocol. We routinely observed that the system determines TGs that are 10-15 decibels off of the optimal TG for our areas of interest which results in a 20-30% error in flip angle.
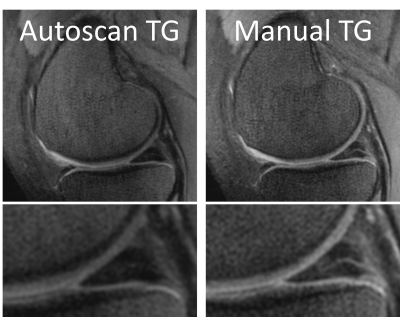
Figure 5. Automatic and Manual Transmit Gain