4359
Intravoxel incoherent motion two-in-one MR sequence for ischemic stroke diagnosis. Initial clinical experience at 3T.1Inserm, UMR 1099, Université de Rennes 1, LTSI, Rennes, France, 2Department of Neuroradiology, Pierre-Zobda-Quitman Hospital, University Hospital of Martinique, French West Indies, France, Fort-de-France, France, 3CRLCC, Centre Eugène Marquis, Rennes, France
Synopsis
This study aims to investigate the feasibility of simultaneously measuring perfusion and diffusion in the acute phase of ischemic stroke with the combined IntraVoxel Incoherent Motion and non-gaussian Diffusional Kurtosis Imaging (DKI-IVIM). For the fifteen patients enrolled, a significant decrease for the diffusion coefficient D and a significant increase in the kurtosis coefficient was observed in the infarcted lesions. Regarding the perfusion, the perfusion fraction f significantly decreased. Enhanced tissues heterogeneity was observable on reconstructed K maps. DKI-IVIM can provide with a clinically acceptable acquisition time both diffusion and perfusion characterization that might be of great interest for stroke diagnosis.
Introduction
In the acute phase of ischemic stroke, two distinct imaging sequences are necessary to reveal the existence of a MRI diffusion-perfusion mismatch. This mismatch delineation is helpful for a safe and effective thrombolytic treatment decision because it can provide the clinically relevant ischemic penumbra estimation.The Intravoxel Incoherent Motion (IVIM) model is a non-invasive method for simultaneous perfusion and diffusion measurements arising from the diffusion signal 1. The diffusional kurtosis imaging (DKI) model enables the characterization of non-Gaussian diffusion providing an additional diffusion parameter, the kurtosis (K), that may better reflect the microstructure heterogeneity 2,3. In this study the DKI-IVIM model that incorporates DKI into the IVIM model has been investigated to assess the feasibility and potential utility of the DKI-IVIM model for both enhanced diffusion characterization and perfusion measurements 5,6 in ischemic stroke.Methods
Fifteen stroke patients (71±11 years old) were enrolled and DKI-IVIM imaging was performed using 9 b-values from 0 to 1500 s/mm2 chosen with the Cramer-Rao-Lower-Bound optimization approach at 3T 4. Sequence parameters were set as following: TR/TE (ms)= 6500/77; Matrix size=128x128; slice thickness=4mm; FOV= 240x240 mm2; NEX=2 for b=1500 s/mm2 with a total of 3 minutes and 9 seconds can duration.IVIM pseudo-diffusion coefficient D*, perfusion fraction f, blood flow-related parameter fD* in addition to the diffusion parameters D (diffusion coefficient) and K were determined in the ischemic lesion and controlateral normal tissue based on a region of interest analysis on the most relevant slices of each patient.The parameters were extracted from the normalized diffusion signal according to the following equation:$$\frac{S(b)}{S_0}=f.e^{-bD^{*}}+(1-f).e^{-bD+\frac{b^2D^2K}{6}}$$.with S0=S b=0 s/mm2. The apparent coefficient diffusion (ADC) and cerebral blood flow (CBF) were also reported from the conventional diffusion and arterial spin labelling (ASL) sequences from the standard stroke imaging protocol for each patient. Statistical analysis of all DKI-IVIM, ADC and CBF parameters were performed using the paired Student t-test and the Pearson correlation test. Motion was also corrected using a two-dimensional (in-plane) image registration algorithm using the $b=0 s/mm^2$ images as reference before data processing. The same parameters were extracted and analyzed with the motion correction application. Moreover, based on a pixel-by-pixel based analysis, parametric maps were also obtained.
Results
The diffusion signals for both ischemic lesions and normal contralateral regions were correctly fitted using the DKI-IVIM model as shown on Figure 1.The paired Student t-test revealed significant differences for all diffusion parameters (Figure 2) with a significant decrease for D (p<0.0001), ADC (p<0.0001), and a significant increase for K (p<0.0001) in the ischemic lesions as reported in the table Figure 3. The perfusion parameter f decreased significantly in the ischemic regions (p=0.0002). The fD* increase was not significant (p=0,56), due to a high variance on this measurement. The paired Student t-test revealed also the same significant differences for all DKI-IVIM parameters except fD* (p =0,47) between ischemic and normal areas with the motion correction.Regarding the conventional diffusion and perfusion parameters, a significant decrease in the ADC values (×10-3 mm2/s) (ADC= 0.49±0.01 vs. ADC=0.78±0.01, p<0,0001) and the CBF (in mL/min/100g) estimated by ASL (CBF=28.3±12,6 vs. CBF=41,0±10,1, p<0.0001) was observed in the lesions.
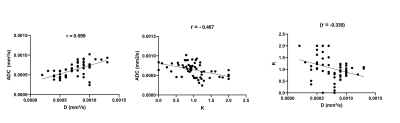
For all patients in both ischemic and controlateral regions, ADC was significantly positively correlated with D ( r =0,599 , p< 0.0001) and negatively with K (r = -0.467, p= 0.0002); K was also significantly correlated with D (r = -0.330, p = 0.01) as reported on Figure 4. An example of reconstructed parametric maps for one patient with the DKI-IVIM is shown on Figure 5.
Conclusion
DKI-IVIM model enables for simultaneous cerebral perfusion and enhanced diffusion characterization in an acceptable clinically acquisition time that might have future clinical implications for the ischemic stroke diagnosis.Acknowledgements
No acknowledgement found.References
1. Le Bihan D, Breton E, Lallemand D, Grenier P, Cabanis E, Laval-Jeantet M (1986) MR imaging of intravoxel incoherent motions: application to diffusion and perfusion in neurologic disorders. Radiology 161:401–407.
2. Jensen JH, Helpern JA (2010) MRI quantification of non-Gaussian water diffusion by kurtosis analysis. NMR Biomed 23:698–710.
3. Wu W-C, Yang S-C, Chen Y-F, Tseng H-M, My P-C (2016) Simultaneous assessment of cerebral blood volume and diffusion heterogeneity using hybrid IVIM and DK MR imaging: initial experience with brain tumors. Eur Radiol. doi: 10.1007/s00330-016-4272-z.
4. Leporq B, Saint-Jalmes H, Rabrait C, Pilleul F, Guillaud O, Dumortier J, Scoazec J-Y, Beuf O (2015) Optimization of intra-voxel incoherent motionimaging at 3.0 Tesla for fast liver examination: Optimization of Liver Motion Imaging at 3.0T. J Magn Reson Imaging 41:1209–1217.
5. De Luca A, Bertoldo A, Froeling M (2016) Effects of perfusion on DTI and DKI estimates in the skeletal muscle: Effects of Perfusion on DTI and DKI in Muscle. Magn Reson Med. doi: 10.1002/mrm.26373.
6. Pavilla, A, Gambarota, G, Arrigo, A, Mejdoubi, M, Duvauferrier, R, & Saint-Jalmes, H. (2017). Diffusional kurtosis imaging (DKI) incorporation into an intravoxel incoherent motion (IVIM) MR model to measure cerebral hypoperfusion induced by hyperventilation challenge in healthy subjects. MagneticResonance Materials in Physics, Biology and Medicine, 1-10.
Figures
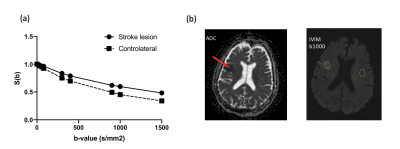
DKI-IVIM analysis on one individual slice of diffusion-weighted images (b = 1000 s/mm ).
(a) Signal intensity plotted as function of b-value for the two ROIs located in the ischemic lesion and normal contralateral region. The slope related to fD* between b = 0s/mm and b = 300 s/mm is decreased for the ischemic region.
(b) Free-hand region of interest (ROI) delineation in the ischemic lesion and the corresponding contralateral ROI on normal tissues.
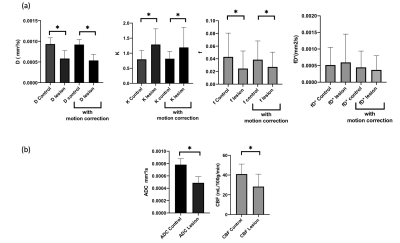
Intravoxel incoherent motion (IVIM) parameters (D, f and fD*) and conventional apparent diffusion coefficient (ADC) and the cerebral blood flow (CBF) mesured through ASL in the lesion and the controlateral normal region averaged over all the stroke patients. Comparison with motion correction data processing for the DKI-IVIM analysis.
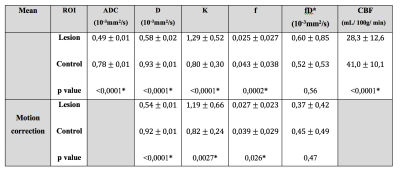
Table.
Comparison of the DKI-IVIM parameters, ADC and CBF between the lesion and the controlateral normal region averaged over all the stroke patients with and without motion correction.
* indicates the statistical significance (p<0.05)