4358
Predictive value of perfusion reduction on ASL for the occurrence of cerebrovascular events in patients with bilateral moyamoya angiography
Maoxue Wang1, Yongbo Yang1, Fei Zhou1, Ming Li1, Jilei Zhang2, and Bing Zhang1,3
1The Affiliated Drum Tower Hospital of Nanjing University Medical School, Nanjing, China, 2Philips Healthcare, Shanghai, China, 3Institute of Brain Science, Nanjing University Nanjing, Nanjing, China
1The Affiliated Drum Tower Hospital of Nanjing University Medical School, Nanjing, China, 2Philips Healthcare, Shanghai, China, 3Institute of Brain Science, Nanjing University Nanjing, Nanjing, China
Synopsis
Predictive value of perfusion reduction on ASL for the occurrence of cerebrovascular events in patients with bilateral moyamoya angiography
introduction
Moyamoya angiography (MMA) is characterized by progressive stenosis of intracranial arteries, followed by neovascular development1. Patients with MMA often present with recurrent stroke because of a decrease in intracranial perfusion. Computed tomography perfusion and dynamic susceptibility contrast are often used to evaluate intracranial perfusion. However, they need a contrast medium. Arterial spin labeling (ASL) imaging is a noninvasive method for evaluating intracranial perfusion without contrast medium2. This study aimed to evaluate the occurrence of cerebrovascular events using ASL in patients with bilateral moyamoya angiography.methods
This study included 27 patients with bilateral MMA (10 male and 17 female, aged 35–66 years), who had stroke or hemorrhage in the unilateral hemisphere. The 3D pseudocontinuous ASL data with two post-labeling delays (PLDs = 1.5 s and 2.5 s) of patients with MMA were collected on an Ingenia 3.0T CX scanner (Philips Healthcare, the Netherlands). The arterial transit artifact (ATA) on cerebral blood flow (CBF) images were assessed with a 4-point grading by two radiologists. The ATAs of bilateral cerebral hemispheres were analyzed using the Wilcoxon symbolic rank test. The mean value, kurtosis, and skewness of the gray distribution of bilateral cerebral hemispheres on CBF images with PLDs of 1.5 s and 2.5 s were calculated on MITK software. The results were analyzed using a paired-sample t test. The relationship between ASL and cerebrovascular events was determined using binary logistics regression analysis.results
No significant difference was found in ATA between bilateral hemispheres on CBF images with PLDs of 1.5 s and 2.5 s. The mean value of CBF in cerebral hemispheres with lesions was lower than that on the contralateral side on CBF images with the PLD of 1.5 s (P < 0.001). The kurtosis and skewness of gray distribution were also significantly different between bilateral cerebral hemispheres (P < 0.05, Table 1). The mean value and skewness of gray distribution of CBF were significantly different between bilateral cerebral hemispheres on CBF images with the PLD of 2.5 s (P < 0.05, Table 1). However, the kurtosis of gray distribution was not significantly different. The mean value of CBF decrease was independently associated with the occurrence of cerebrovascular events (P < 0.05) in patients with MMA (Table 2).conclusion
The mean value of CBF in cerebral hemispheres with lesions was lower than that on the contralateral side in ASL with PLDs of 1.5 s and 2.5 s, and it was correlated with the occurrence of cerebrovascular events. The perfusion decrease on ASL may serve as an independent predictor of cerebrovascular events in patients with bilateral MMA.Acknowledgements
This work was supported by the National Natural Science Foundation of China (81720108022 B.Z., 81971596, X.Z., 82071904, Z.Q.); Supported by the Fundamental Research Funds for the Central Universities, Nanjing University (2020-021414380462); The key project of Jiangsu Commission of Health (K2019025); Key medical talents of the Jiangsu province, the "13th Five-Year" health promotion project of the Jiangsu province (ZDRCA2016064); Jiangsu Provincial Key Medical Discipline (Laboratory) (ZDXKA2016020); the project of the sixth peak of talented people (WSN -138).References
1. Herve D, Kossorotoff M, Bresson D, et al. French clinical practice guidelines for Moyamoya angiopathy. Rev Neurol (Paris),2018, 174(5): 292-303.
2. Nam KW, Kim CK, Ko SB, et al. Regional arterial spin labeling perfusion defect is associated with early ischemic recurrence in patients with a transient ischemic attack. Stroke,2020, 51(1): 186-192.
Figures
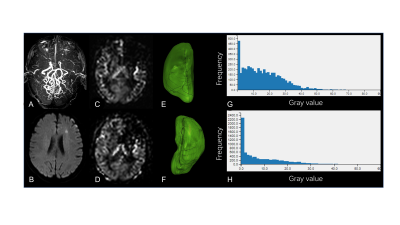
Figure 1. A 61-year-old patient with bilateral MMA. (A)
Occlusion of bilateral ICA, ACA, and MCA was observed on 3D time of flight MRA
images. (B) He had a punctate acute cerebral infarction in the left frontal
lobe. The
perfusion of the left frontal lobe decreased, and the arterial transit artifact
was grade 2 on CBF images when PLD were 1.5 s and 2.5 s (C and D). (E and F) Three-dimensional
images of bilateral cerebral hemispheres. The gray value of the left cerebral
hemisphere was less than that of the contralateral on the gray distribution
histogram of bilateral cerebral hemispheres.
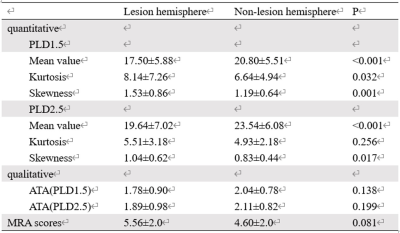
Table 1. Quantitative and qualitative parameters of
ASL and the degree of vascular stenosis in bilateral cerebral hemispheres in
patients with moyamoya angiography.
ATA, Arterial transit artifact.
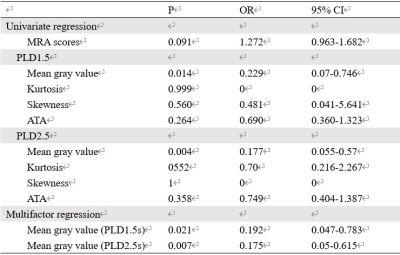
Table 2. Correlation between the degree of
intracranial artery, cerebral perfusion, and occurrence of cerebrovascular
events in patients with MMA.