4350
4D Flow MRI assessment of cerebral blood flow before and after superficial temporal artery-middle cerebral artery bypass surgery1Center for Biomedical Imaging Research, Department of Biomedical Engineering, Tsinghua University, Beijing, China, 2Department of Neurosurgery, West China Hospital, Sichuan University, Chengdu, China
Synopsis
In this study, we utilized 4D Flow MRI to assessed and compared the change of cerebral blood flow in patients with MMD before and after STA-MCA bypass surgery. Statistics indicated that BFVtotal significantly increased after bypass surgery while no differences were found in BFViICA, BFVcICA and BFVBA. This is probably because the STA-MCA bypass could directly compensate for blood flow supply and play a role in flow augmentation for the whole brain. The results of this study suggested that STA-MCA bypass could improve the cerebral blood supply without affecting the hemodynamics of other arteries, such as BA and ICA.
Introduction
Moyamoya disease (MMD) is a cerebrovascular disease characterized by chronic progressive stenosis and/or occlusion of unilateral or bilateral internal carotid arteries, anterior cerebral artery, and middle cerebral artery.1,2 Surgical revascularization is believed to be the most effective therapy to improve the cerebral blood supply and prevent ischemic or hemorrhagic stroke for moyamoya disease.3-5 However, no direct evidence including quantitative information such as blood flow volume (BFV) has been provided to verify the hemodynamic change pre- and postoperation of revascularization. In this work, 4D Flow MRI was used to acquire more detailed information about how bypass surgery impacts cerebral hemodynamics.Methods
Study Population: A total of 14 patients (6 males and 8 females, age range: 9 ~ 69 years) with MMD who underwent superficial temporal artery-middle cerebral artery (STA-MCA) bypass were included in this study. Written informed consents were obtained from all patients.MR Experiments: In addition to clinical MRI sequences including diffusion-weighted imaging, time-of-flight MRA (TOF-MRA), 4D Flow MRI were performed on a 3.0T MRI scanner (Magnetom Symphony, Siemens Healthcare, Erlangen, Germany) preoperatively and 1 week after bypass surgery (mean 7.6 d, range 6-11 d after surgery). 4D Flow MRI was used for hemodynamic evaluation. Scan parameters were: TR/TE = 46.8/2.8 ms, flip angle = 10°, FOV = 169 x 200 x 32 mm3, voxel size = 0.78 x 0.78 x 1 mm3. The value of VENC was set appropriately for each patient based on the results of the pre-scan.
Data Analysis: The velocity data were generated from a 4D Flow MRI data set using GT Flow software (Ver. 3.10, GyroTools, Zurich, Switzerland). The BFV of the ipsilateral ICA (BFViICA), contralateral ICA (BFVcICA), BA (BFVBA), and bypass artery (BFVBypass) were measured using the semiautomatic iso-contour mode on the plane of the target vessel, which were resliced perpendicularly to the target artery. The same location was chosen to measure for each artery.
Statistical analysis: To verify whether the bypass artery could compensate for the BFV of other cerebral arteries, the difference of BFViICA, BFVcICA, BFVBA between preoperation and postoperation were evaluated by paired sample t-test. To investigate whether the bypass artery could improve the cerebral blood supply, total BFV (BFVtotal) was also compared before and after surgery using paired sample t-tests. BFVtotal was calculated using the following formula:
$$BFV_{total} = BFV_{iICA} + BFV_{cICA} + BFV_{BA} (preoperative) $$
$$ = BFV_{iICA} + BFV_{cICA} + BFV_{BA} + BFV_{bypass} (postoperative) $$
The level of statistical significance was set at p < 0.05. All statistical analysis were conducted by MedCalc (MedCalc Software, Mariakerke, Belgium).
Results
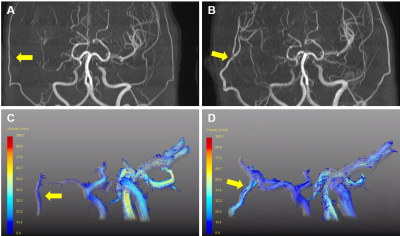
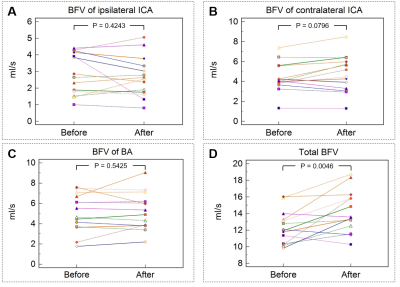
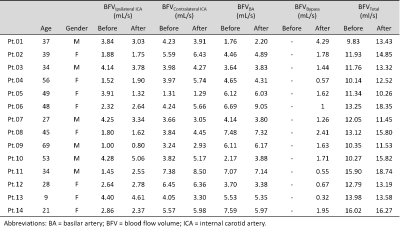
Patency of the bypass artery was confirmed visually in all patients using 4D Flow MRI, as shown in Figure.1. Figure.2 and Table.1 showed the change of BFViICA, BFVcICA, BFVBA and BFVtotal of all patients before and after bypass surgery, and individual patient data were summarized in Table.1. Furthermore, the results of paired samples t-test indicated that the total BFV (p = 0.0046) significantly increased after revascularization. There is no difference of BFViICA (p = 0.4243), BFVcICA (p = 0.0796) and BFVBA (p = 0.5425) before and after STA-MCA bypass, as shown in Table.1.Discussion and Conclusion
In this study, we assessed and compared the change of cerebral blood flow in patients with MMD before and after STA-MCA bypass surgery. Statistics indicated that BFVtotal significantly increased after bypass surgery, while slight but not significant decrease was found in BFViICA, at the meantime slight but not significant increase was found in BFVcICA and BFVBA. This is probably because the STA-MCA bypass could directly compensate for blood flow supply for the whole brain while have no impact on the hemodynamics of circle of Willis6. Previous research showed that STA-MCA bypass played a role in flow augmentation7, which is consistent with our findings.In conclusion, the results of this study by 4D Flow MRI suggested that STA-MCA bypass could directly improve the cerebral blood supply without affecting the hemodynamics of other arteries, such as BA and ICA.
Acknowledgements
No acknowledgement found.References
1. Suzuki J, Kodama N. Moyamoya disease--a review. Stroke. 1983 Jan-Feb;14(1):104-9.
2. Kuroda S, Houkin K. Moyamoya disease: current concepts and future perspectives. Lancet Neurol. 2008 Nov;7(11):1056-66.
3. Ishikawa T, Houkin K, Kamiyama H, et al. Effects of surgical revascularization on outcome of patients with pediatric moyamoya disease. Stroke. 1997 Jun;28(6):1170-3.
4. Fung LW, Thompson D, Ganesan V. Revascularisation surgery for paediatric moyamoya: a review of the literature. Childs Nerv Syst. 2005 May;21(5):358-64.
5. Guzman R, Lee M, Achrol A, et al. Clinical outcome after 450 revascularization procedures for moyamoya disease. Clinical article. J Neurosurg. 2009 Nov;111(5):927-35.
6. Chen Y, Xu W, Guo X, et al. CT perfusion assessment of Moyamoya syndrome before and after direct revascularization (superficial temporal artery to middle cerebral artery bypass). Eur Radiol. 2016 Jan;26(1):254-61.
7. Kuroda S, Houkin K, Ishikawa T, et al. Novel bypass surgery for moyamoya disease using pericranial flap: its impacts on cerebral hemodynamics and long-term outcome. Neurosurgery. 2010 Jun;66(6):1093-101.
Figures