4348
Longitudinal analysis revealed increased parenchymal free water may be relieved by revascularization surgery in patients with moyamoya disease1Neurosurgery, Tokyo Medical and Dental University, Tokyo, Japan, 2Radiology, Juntendo University, Tokyo, Japan, 3Radiology, Toho University Omori Medical Center, Tokyo, Japan
Synopsis
To investigate specific microstructural change after the revascularization surgery, we evaluated 13 patients with moyamoya disease and 13 age-sex matched normal controls using multishell diffusion MRI. By NODDI and free-water imaging analysis, preoperative hemispheres showed significant increase of extracellular fluid compared to controls, and subsequent significant decrease after the surgery. Only free-water eliminated parameter (orientation dispersion index) showed significant difference between patients with and without cognitive improvement after the surgery. Increased parenchymal free water observed in moyamoya disease may decrease after the surgery, and free-water elimination might be useful to detect true neuronal change related to postoperative cognitive improvement.
Background and Purpose
Conventional diffusion MRI parameters such as fractional anisotropy (FA) is reported to be altered in patients with moyamoya disease compared to normal controls, and to change significantly after the revascularization surgery1-3. However, the specific histological change underlying these postoperative parametrical changes -i.e. whether they results from the extracellular free water or the true neuronal structure - remains unclear. To clarify this point, we applied two diffusion analysis, i.e. neurite orientation dispersion and density imaging (NODDI)4 and free water imaging using bi-tensor model5 in patients with moyamoya disease and normal controls, and also investigate whether microstructural parameters relates to postoperative cognitive improvement.Material and Methods
ParticipantsThis prospective study was approved by ethical committee of local institutes. Thirteen patients with moyamoya diasese (11 females; aged 16–55 years (average, 37.9) participated in this study. Patients were evaluated with MRI and cognitive test, before and one year after the surgery. During the same period, 13 age- and sex-matched normal subjects (11 females, aged 17-56 years (average, 38.4)) were evaluated by the same MRI protocol as well.
Cognitive assessments
Working Memory Index measured with Weschler Adult Intelligence Scale is regarded as frontal lobe function declined in adult patients with moyamoya disease, was used to define cognitive decline and improvement. Working Memory Index lower than standard deviation of normal controls was defined as cognitive decline, and the increase of the scores more than 90% confidence interval of normal controls6. Of all, seven (54%) patients showed preoperative cognitive decline, and five (38%) patients showed postoperative cognitive improvement.
Diffusion analysis
All MRI data were acquired using a 3 T system (MAGNEOM Skyra, Siemens, Germany) equipped with a 32 multichannel receiver head coil. Diffusion-weighted images were acquired using a fat-saturated single-shot echo planar imaging sequence (b values and axes=0, 700: 30 axes, 2850: 60 axes. Postprocessing of data was conducted using MATLAB 2016a (MathWorks Inc., Natick, MA, USA) and SPM12. The reversed phase image was also acquired and used to estimate the susceptibility-induced off-resonance field to correct the deformation using FMRIB Software Library version 5.0.9 (FSL)7. Then the data was fitted to the NODDI model using the NODDI MATLAB toolbox version 0.94 and converted to intracellular volume fraction (Vic), orientation dispersion index (OD) and isotropic volume fraction (Viso). The same data were also used to fit to a regularized bi-tensor model5 by in-house script to create free water fraction (FWF) and FW-corrected fractional anisotropy (FAt). Conventional fractional anisotropy (FA) was also created from single shell data (b=0 and 700) using DTIFIT tool implemented in FSL.
Calculation of Regional values and statistical analysis
After removal of extracellular signals from each map and spatial normalization, standard vascular atlas8 was used to calculate gray and white matter value of anterior cerebral artery (ACA), middle cerebral artery (MCA) and posterior cerebral artery (PCA) territories. Paired T test was performed to evaluate preoperative and postoperative regional values, and unpaired T test was performed to evaluate regional values between patients with and without postoperative cognitive improvement. P<0.05 (after Bonferroni correction for comparing six parameters) was regarded as statistically significant.
Results
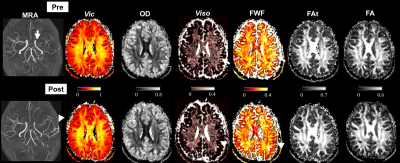
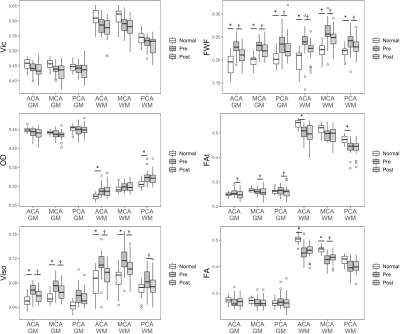
Representative parametrical maps are shown in Fig. 1.Compared to normal controls, preoperative regions of patients with moyamoya disease showed significantly higher Viso and FWF in most gray and white matter regions (Fig. 2). In the white matter of ACA and PCA, preoperative OD values showed significantly higher, and preoperative FAt showed significantly lower values compared to normal controls. Conventional FA values of preoperative patients in the white matter of ACA and MCA showed significantly lower values than normal controls, and MCA values showed significant increase after surgery.
After the revascularization surgery, Viso and FWF showed significant decrease in most regions, and FA showed significant increase in the white matter of MCA.
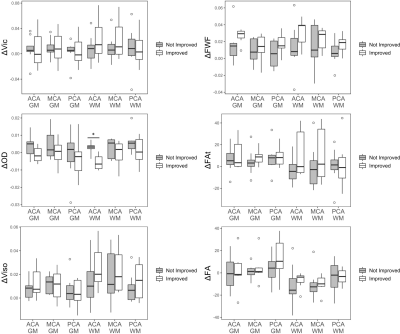
When comparing patients with and without cognitive improvement after the surgery, patients with cognitive improvement showed significant decrease of OD in the white matter of ACA (Fig. 3).
Discussion
Previous studies evaluating various neurological diseases suggested altered conventional diffusion parameters like FA are largely determined by extracellular fluid increase rather than alterations of white matter fiber organization9-10. Our study also suggests altered conventional diffusion parameters in patients with moyamoya disease may comes from the extracellular fluid change, rather than the neuronal network itself.Although previous studies evaluated cognitive performance and conventional diffusion parameters after the revascularization surgery, direct relationship between them have never been reported1-3. We also did not find direct relationship between the postoperative change of FA and cognitive improvement, and only found OD values in the white matter ACA might relate to cognitive improvement. Lack of direct relationship between conventional diffusion parameters and cognitive performance may due to the extracellular fluid affecting the conventional diffusion parameters.
Acknowledgements
We thank the Department of Radiology in Tokyo Medical Clinic for magnetic resonance imaging acquisition.References
1. Qiao P-G, Cheng X, Li G-J, et al. MR Diffusional Kurtosis Imaging–Based Assessment of Brain Microstructural Changes in Patients with Moyamoya Disease before and after Revascularization. American Journal of Neuroradiology 2020
2. Kazumata K, Tha KK, Tokairin K, et al. Brain Structure, Connectivity, and Cognitive Changes Following Revascularization Surgery in Adult Moyamoya Disease. Neurosurgery 2019;85:E943-E952
3. Calviere L, Loubiere P, Planton M, et al. Decreased frontal white-matter diffusion and improved cognitive flexibility after burr-hole surgery in moyamoya angiopathy. BMC Neurology 2020;20:30
4. Zhang H, Schneider T, Wheeler-Kingshott CA, et al. NODDI: practical in vivo neurite orientation dispersion and density imaging of the human brain. Neuroimage 2012;61:1000-1016
5. Pasternak O, Sochen N, Gur Y, et al. Free water elimination and mapping from diffusion MRI. Magn Reson Med 2009;62:717-730
6. Fujita K, Maekawa H, Dairoku H, et al. Assessment cases and clinical researches using Japanese version of WAIS-III. Nihon Bunka Kagakusha; 2011
7. Jenkinson M, Beckmann CF, Behrens TE, et al. Fsl. Neuroimage 2012;62:782-790
8. Mutsaerts HJ, van Dalen JW, Heijtel DF, et al. Cerebral Perfusion Measurements in Elderly with Hypertension Using Arterial Spin Labeling. PLoS One 2015;10:e0133717
9. Chad JA, Pasternak O, Salat DH, et al. Re-examining age-related differences in white matter microstructure with free-water corrected diffusion tensor imaging. Neurobiology of aging 2018;71:161-170
10. Andica C, Kamagata K, Hatano T, et al. Free-Water Imaging in White and Gray Matter in Parkinson's Disease. Cells 2019;8
Figures