4343
Accuracy of Intravoxel Incoherent Motion (IVIM) for quantification of perfusion-diffusion mismatch in Acute Stroke.1The University of Chicago, Chicago, IL, United States, 2Northwestern University, Chicago, IL, United States, 3University of Illinois at Chicago, Chicago, IL, United States
Synopsis
This is a retrospective validation study of intravoxel incoherent motion (IVIM) over a range of physiologic conditions: normocapnia, hypercapnia, and post middle cerebral artery occlusion. We performed controlled two-day experiments in a canine model (n=17) of ischemic stroke with baseline (normocapnia) and hypercapnia on the first day followed by occlusion on the second. We compared IVIM perfusion and diffusion images with neutron capture microsphere perfusion, DSC perfusion, and Apparent Diffusion Coefficient (ADC) from standard DWI. We found excellent agreement between IVIM for both perfusion and diffusion indicating IVIM may serve as a means of stratifying acute stroke patients for treatment.
INTRODUCTION
MRI perfusion imaging is important in diagnosis, treatment, and prognosis of neurological diseases. IVIM is a well-established technique(1) for extracting both perfusion and diffusion weighted images. Using our previously developed scan protocol and image post-processing algorithm we quantify cerebral perfusion (i.e. cerebral blood flow in mL/100g/min) with IVIM images and compare the results to reference standard quantitative DSC CBF(2,3) and neutron-capture microsphere deposition(4). IVIM diffusion measurement was compared to ADC infarct volume with an automatic threshold post-occlusion.The goal of this work is to test the hypothesis that quantification of IVIM perfusion is correlated with standard quantitative CBF over a range of physiologic states, and that IVIM diffusion is correlated with standard ADC infarct volume in stroke. We hypothesize that quantitative IVIM perfusion and diffusion correlate with reference standard “truth” values, with the benefit of being completely non-invasive.
METHODS
Experimental Model: All MRI scans were performed on a 3T MRI scanner (Achieva, Philips) using a 15 channel receive only coil. A series of n=17 mongrel canine experiments were normocapnic and anesthesia was achieved by isoflurane (1% end-tidal, 0.75 MAC), continuous propofol infusion (100-200 μg/kg/min), and intravenous rocuronium (0.4-0.6 mg/kg) to maintain normal cerebral perfusion. In a series of two-day experiments, subjects were scanned at normocapnia (ETCO2 ~ 30 mmHg), hypercapnia (7% carbogen respiration, ETCO2 ~ 60 mmHg) and on day two, post middle cerebral artery occlusion(5). ETCO2 was continually monitored and but quantified with direct arterial blood sampling from the aorta at the time of MRI measurement.DSC Perfusion/Diffusion: Quantitative DSC CBF images were acquired within 5 minutes of the IVIM scans. Multi-phase, single shot EPI, FOV/matrix = 160/128, 5 2.0 mm thick slices, 50 measurements, with a 3 ml iv Gd with fast T1 maps were acquired before and after the contrast scan. Standard ADC maps were acquired within 30 minutes of IVIM scans post occlusion and infarct volume was calculated comparing volume of ADC and D values below a certain threshold.
Microsphere Perfusion: Neutron-capture microsphere quantitative CBF was acquired in a subset of cases with microspheres injected within 5 minutes of MRI sequences. Each injection consisted of 4mL of stable-isotope labeled 15μm microspheres (STERIspheres, BioPal Inc, Medford, MA) into the left ventricle over 10s. 20mL of blood at 10 mL/min was withdrawn for analysis while reference blood was withdrawn from the abdominal aorta with an MRI compatible withdraw pump(PHD 2200, Harvard Apparatus, Holliston, MA, USA). Slices were then analyzed through neutron activation (Biopal, Worcester, MA, USA).
IVIM Analysis: IVIM images were acquired with ten b-values (0,111, 222, 333, 444, 556, 667, 778, 889, 1000), and 3 directions of DWI images were acquired to cover the whole head (slices/thickness= 2mm, FOV = 14764mm, total scan time =332s ). The IVIM data normalized to b0-value was fit to a bi-exponential model $$$\frac{S(b)}{S(b=0)}= fe^{(D^*\times b )}+(1-f)e^{(D\times b)}$$$ to yield 2D parametric images of $$$ qCBF = \frac{6f_w}{\rho L \langle l \rangle}f\times D^* $$$ and diffusion coefficient images $$$ D $$$. The quantification factor was calculated using values previously determined by Wirestam et al (6). The bi-exponential fit was performed using a two-step algorithm, developed in-house using Python by subtracting the fit of the diffusion regime (b> 200 s/mm2) and fitting the perfusion component to the remainder.
CVR Analysis: Cerebrovascular reserve (CVR) is linearly related to the degree of hemodynamic failure in carotid artery disease and a predictor of impending stroke in neurovascular disease. In this study CVR was calculated from $$$ CVR = \frac{CBF_C-CBF_B}{CBF_B}\times \frac {100}{\Delta CO_2} $$$ with $$$ CBF_B $$$ as normocapnic CBF and $$$ CBF_C $$$ as hypercapnic CBF for both IVIM perfusion and DSC qCBF. For all images regions of interest were compared using standard scatter plots.
RESULTS
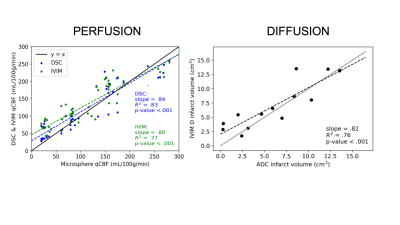
Figure 1 shows representative images of DSC perfusion (top row) at normocapnia, hypercapnia and after MCAO occlusion. The corresponding IVIM images are shown below. DWI ADC image and IVIM D shown indicate SNR and resolution are comparable to reference standard prefusion-diffusion mismatch images.Correlation of quantitative IVIM perfusion and DSC qCBF was found $$$ (m=.72, r^2 = .67, p = 1.5e^{-34}) $$$ for eleven cases over three physiologic states supporting significant correlation between IVIM and DSC. A subset of four cases of both IVIM and DSC qCBF were compared to neutron-capture microspheres seen in Figure 2a and returned $$$ (m=.80, r^2 = .77, p = 1.4e^{-18}) $$$ and $$$ (m=.84, r^2 = .83, p = 7.4e^{-20}) $$$. There is a similarly strong correlation between IVIM D and ADC $$$ (m=.82, r^2 = .76, p = 1.1e^{-4}) $$$ for thirteen cases post-MCAO seen in Figure 2b. CVR calculated by IVIM was shown to be strongly correlated with DSC CVR value $$$ (m=1.15, r^2 = .85, p = .009) $$$.
DISCUSSION AND CONCLUSION
We found IVIM perfusion values correlate strongly with reference standards values for both imaging, DSC qCBF and ADC, and direct tissue pathology by neutron-capture microspheres, over a range of values and physiologic conditions such as normocapnia, hypercapnia, and occlusion. Both CVR and infarct volume measured with IVIM are in strong agreement with reference values, which support the development of IVIM measured perfusion for clinical use.Acknowledgements
Research reported in this publication is supported by the NIH Grant R01NS093908 and the NSF Grant DGE-1746045.References
1. Le Bihan D, Breton E, Lallemand D, Grenier P, Cabanis E, Laval-Jeantet M. MR imaging of intravoxel incoherent motions: application to diffusion and perfusion in neurologic disorders. Radiology 1986;161(2):401-407.
2. Mouannes-Srour JJ, Shin W, Ansari SA, Hurley MC, Vakil P, Bendok BR, Lee JL, Derdeyn CP, Carroll TJ. Correction for arterial-tissue delay and dispersion in absolute quantitative cerebral perfusion DSC MR imaging. Magn Reson Med 2012;68(2):495-506.
3. Carroll TJ, Horowitz S, Shin W, Mouannes J, Sawlani R, Ali S, Raizer J, Futterer S. Quantification of cerebral perfusion using the "bookend technique": an evaluation in CNS tumors. Magn Reson Imaging 2008;26(10):1352-1359.
4. Jeong YI, Christoforidis GA, Saadat N, Kawaji K, Cantrell CG, Roth S, Niekrasz M, Carroll TJ. Absolute quantitative MR perfusion and comparison against stable‐isotope microspheres. Magn Reson Med 2019;0(0):1-11.
5. Christoforidis GA, Rink C, Kontzialis MS, Mohammad Y, Koch RM, Abduljalil AM, Bergdall VK, Roy S, Khanna S, Slivka AP, Knopp MV, Sen CK. An endovascular canine middle cerebral artery occlusion model for the study of leptomeningeal collateral recruitment. Invest Radiol 2011;46(1):34-40.
6. Wirestam R, Borg M, Brockstedt S, Lindgren A, Holtas S, Stahlberg F. Perfusion-related parameters in intravoxel incoherent motion MR imaging compared with CBV and CBF measured by dynamic susceptibility-contrast MR technique. Acta Radiol 2001;42(2):123-128.
Figures
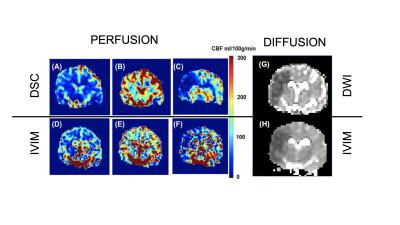
Figure 1: Shown on the left are quantitative DSC CBF (A,B,C) and quantitative IVIM perfusion (D,E,F) images at normocapnia, hypercapnia, and post-occlusion. On the right is a standard ADC map (G) compared to IVIM diffusion coefficient image (H) post-occlusion.