4338
Cerebral circulation time related DMN connectivity in intracranial dural arteriovenous fistula before and after treatment1Imaging Sciences and Interventional Radiology, Sree Chitra Tirunal Institute for Medical Sciences and Technology, Thiruvananthapuram, India, 2Neurology, Sree Chitra Tirunal Institute for Medical Sciences and Technology, Thiruvananthapuram, India
Synopsis
Cognitive decline is a common non-hemorrhagic complication of intracranial dural arteriovenous fistula (DAVF). Increase in cerebral circulation time (CCT) can be related to significant resting-state functional changes in the brain. 30 DAVF patients and a similar cohort of age-matched controls underwent resting-state functional MRI (rsfMRI) and the results were correlated with CCT and neuropsychological profile. Patients with high CCT showed decreased connectivity at DMN seed regions and less compensatory pre-frontal connectivity (pFDR < 0.05), which showed a trend in reversal after a month of embolisation therapy. These findings may be of significance in formulating treatment strategies in DAVF.
Introduction
Clinical or sub-clinical cognitive impairment is well-known in intracranial dural arteriovenous fistula (DAVF) which is potentially reversal after treatment 1. Venous congestion and local or global venous hypertension are major contributing factors of cognitive decline in DAVF1,2. Cerebral circulation time (CCT) is a direct angiographic measure of cerebrovascular reserve and indicates the severity of venous hypertension & venous congestion in intra-cranial DAVF 3,4. We studied cerebral circulation time-related resting-state functional magnetic resonance imaging (rsfMRI) changes in default mode network (DMN) connectivity and its association with cognitive decline in intracranial DAVF. Post embolization follow up rsfMRI changes after a month were also studied.Methods
Baseline(pre) and 1-month post-embolization rsfMRI were performed in 30 dural arterio-venous fistula patients (DP) and 30 age, and gender-matched healthy controls (HC). Images were acquired on a 3T MRI scanner (GE Discovery MR750w) with its standard 32 channel head array coil. All patients underwent digital subtraction angiography (DSA) with GE Innova biplane 3131 digital subtraction equipment (generator of 1000 KW, RDL standard auto exposure). rsfMRI images were processed and analyzed using Conn Connectivity toolbox. The functional connectivity analysis between the region of interest (ROI) was done using group independent component analysis (ICA) and ROI to ROI analysis (pFDR corrected < 0.05). Pre and post embolization mean cerebral circulation time (CCT) was calculated from DSA images using the average of median values of right anterior, left anterior and posterior circulations times. A cut off value of 5.833 seconds, was used to categorize patients into those with high and low CCT. Neuropsychological scores between high and low CCT patients were compared and correlated with functional connectivity changes.Results
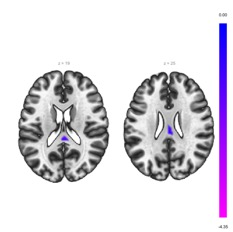
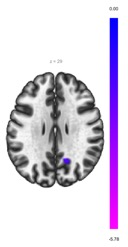
In group ICA analysis, the patient group with high CCT showed significantly decreased connectivity in the precuneus -posterior cingulate (PC-PCC) seed region of DMN (pFDR corrected < 0.01) unlike low CCT (pFDR corrected=0.049) in comparison to HC. In ROI-to-ROI analysis, the patient group with high CCT showed less prominent to absent increased connectivity between PCC of DMN with pre-frontal cortex and cerebellum as compared to low CCT (pFDR<0.01), suggests a compensatory failure in the high CCT group. Further, in the high CCT group, decreased connectivity between DMN and amygdala (pFDR<0.01) was noted. The neuropsychological profile showed high CCT group with lower scores as compared to low CCT (p<0.05), suggesting significant cognitive decline in the high CTT group. Post embolisation at 1 month follow up showed improvements in connectivity changes and neuropsychological scores compared to embolisation status(p<0.05).Discussion
Increase in cerebral circulation time is noted in high grade DAVF and is related to cognitive decline in DAVF patients. This study explored the correlates of CCT to rsfMRI changes in DMN at PC-PCC and its connectivity to pre-frontal regions. It was found that cognitive decline and increased CCT in DAVF patients were well correlated to rsfMRI network changes and were reversibile after embolization treatment. Treatment strategy in DAVF is currently decided by the clinical presentation of the patient and the grade of the fistula and is primarily aimed at preventing cerebral hemorrhage. Since embolothearpy is not without risk of developing complications, the strength of CCT to DMN functional connectivity changes might be of significance in formulating objective treatment guidelines in DAVF patients to prevent or reverse cognitive decline in them.Conclusion
Reversible cognitive decline in DAVF is related to the changes in circulation time and is correlated to corresponding rsfMRI network modulations. This may be of significance in formulating treatment decision strategies.Acknowledgements
The authors would like to acknowledge the financial support for this study by the following projects:
TDF project 6107/ 2018, SCTIMST, Department of Science and Technology, Govt: of India
DST/CSRI/2018/11, Department of Science and Technology, Govt: of India
References
1. Wilson M, Doran M, Enevoldson TP, Larner AJ. Cognitive profiles associated with intracranial dural arteriovenous fistula. Age and ageing. 2010;39(3):389-92.
2. Enofe I, Thacker I, Shamim S. Dural arteriovenous fistula as a treatable dementia. InBaylor University Medical Center Proceedings 2017 (Vol. 30, No. 2, pp. 215-217).
3. Yamamoto S, Watanabe M, Uematsu T, Takasawa K, Nukata M, Kinoshita N. Correlation of angiographic circulation time and cerebrovascular reserve by acetazolamide-challenged single photon emission CT. American Journal of Neuroradiology. 2004 ;25(2):242-7.
4. Deguchi J, Yamada M, Kobata H, Kuroiwa T. Regional cerebral blood flow after acetazolamide challenge in patients with dural arteriovenous fistula: simple way to evaluate intracranial venous hypertension. American journal of neuroradiology. 2005;26(5):1101-6.