4330
Distinct Effects on Cognition Caused by the Side of Asymptomatic Carotid Artery Stenosis1National Yang-Ming University, Taipei, Taiwan, 2School of Medicine, National Yang-Ming University, Taipei, Taiwan, 3Neurological Institute, Taipei Veterans General Hospital, Taipei, Taiwan, 4Institute of Brain Science, National Yang-Ming University, Taipei, Taiwan
Synopsis
Previous studies reported that the patients with asymptomatic internal carotid stenosis (aICS) had a higher risk of stroke and neurocognitive impairment. However, whether the side of aICS could cause different neurocognitive outcomes was less explored. In this study, significant difference of functional connectivity (FC) was found between the left and right aICS groups. The association between FC and neuropsychological measures (dizziness, immediate and delayed recall verbal memory) revealed by the correlation analysis also presented different profiles between two aICS groups.
Background and Purpose
The patients with asymptomatic internal carotid stenosis (aICS) have a higher risk of ischemic stroke.[1] In addition to vascular events, previous studies have pointed out that the patients with aICS may also suffer from dizziness and cognitive impairment (verbal memory), which were possibly attributed to the impaired perfusion.[2] However, the comparison of functional connectivity (FC) and corresponding symptoms between left and right aICS was less explored. In this study, we aimed to investigate whether the laterality of aICS is a factor associated with the organization of FC and the type/extent of presented neurocognitive symptoms. We hypothesized that the association between the FC and neuropsychological measures would be different between left and right aICS groups.Materials and Methods
We recruited 36 healthy controls (HCs), 26 patients with left aICS (aICSL), and 40 patients with right aICS (aICSR). Inclusion criteria of patients were the degree of stenosis greater than 60%, and no neurodegenerative diseases. Dizziness handicap inventory (DHI) and verbal memory test were used to evaluate the severity of dizziness and level of working (immediate) and short-term (delayed recall) memory, respectively (Table 1).[3] MRI data, including 3D BRAVO T1-weighted images (TR/TE: 12.2/5.2 ms; voxel size: 1.0×1.0×1.0 mm3) and EPI BOLD fMRI (TR/TE: 3000/30ms; voxel size: 1.73×1.73×3mm3) during resting state (124 volumes) were acquired on a 3T MR scanner (GE, Discovery 750).The fMRI data were preprocessed with the standard procedures using Data Processing Assistant for Resting-State fMRI (DPARSF) toolbox.[4] The preprocessing procedures included the correction for slice timing, realignment, co-registration of 3D-T1W images to BOLD fMRI, regression out confounding effects of motion parameters and signals from white matter and cerebrospinal fluid, spatial normalization, and spatial smoothing with a 6-mm full-width half-maximum Gaussian kernel. The cortical and subcortical regions were parcellated into 116 regions based on the Automatic Anatomical Labeling atlas (AAL116).[5] The FC was estimated by calculating Pearson’s correlation coefficient between each pair of regional BOLD signals (with a bandpass filtering between 0.01 and 0.10 Hz) followed by the Fisher’s r-to-z transform.
Two-sample t-test was used to identify the significant differences of FC between aICSL and aICSR groups (p<0.05). Correlation analysis was performed to further reveal the associations between FC and neuropsychological measures (p < 0.05). The processing workflow is shown in Figure 1.
Results and Discussion
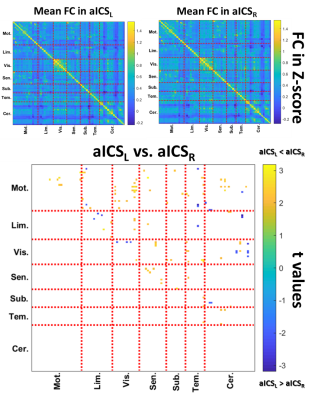
The patients with aICS had significantly more severe dizziness and deficit on verbal memory test compared to the HCs (Table 1). For the comparison between aICSL and aICSR groups, the recall verbal memory was significantly poorer in the aICSL than in the aICSR group (Table 1).Figure 2 shows the significant differences of FC matrices between aICSL and aICSR groups. In the aICSR group, several significantly stronger FC (positive t values labelled by yellow in Figure 2) were found within motor areas, between motor and visual areas, and cerebellum areas compared to the aICSL group. Few significant lower values of FCs (negative t values labelled by blue in Figure 2) were observed within visual areas and between visual and cerebellum areas in the aICSR group. Results showed that patients with aICSL tended to have reduced FC in most of significantly different connectivity compared to the aICSR group.
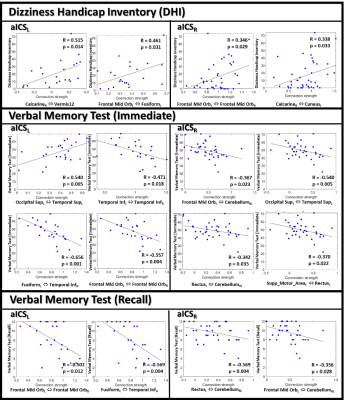
To further investigate the association between the altered FC and neuropsychological assessments (DHI, immediate verbal memory, and recall verbal memory), we displayed scatter plots with significant correlations for the aICSL and aICSR group, respectively (Figure 3). In general, the aICSL group exhibited stronger correlations (higher absolute correlation coefficients) between FC and neuropsychological assessments compared to the aICSR group. For example, the FC between the right calcarine and vermis12 showed a positive correlation (R=0.515) with dizziness score, indicating that a stronger FC may accompany a higher degree of dizziness. Calcarine is involved in the visual function, and the function of vermis is related to posture control. Accordingly, the alteration of FC between the right calcarine and vermis12 may be associated with vertigo after aICSL.[6] The FC between the left fusiform and right inferior temporal gyrus also showed negative correlations with immediate verbal memory (R=-0.656) and recall verbal memory (R=-0.569) in the aICSL group. Fusiform is directly related to textual cognition. Inferior temporal handles the object identification by comparing the processed information to stored memories of objects. With the trigger of stored memory, the FC between the right fusiform and left inferior temporal may compensate the cognitive impairment (working and short-term memory) in aICSL.
Conclusions
In this study, we reported that patients with aICSL showed poorer performance in the recall verbal memory and significant decreased FC analysis compared to patients with aICSR. Different profiles of association between FC and neuropsychological assessments were found between two aICS groups. Based on our results, the laterality of aICS can be one of the key factors to link with the decline of verbal memory function and guide the treatment for patients with aICS.Acknowledgements
This work was supported by the Ministry of Science and Technology, Taiwan (MOST 109-2314-B-010-022-MY3) and the National Yang-Ming University (VGHUST110-G7-2-2).References
1. Abbott, A.L., et al., Systematic Review of Guidelines for the Management of Asymptomatic and Symptomatic Carotid Stenosis. Stroke, 2015. 46(11): p. 3288-301.
2. Cheng, H.L., et al., Impairments in cognitive function and brain connectivity in severe asymptomatic carotid stenosis. Stroke, 2012. 43(10): p. 2567-73.
3. Jacobson, G.P. and C.W. Newman, The development of the Dizziness Handicap Inventory. Arch Otolaryngol Head Neck Surg, 1990. 116(4): p. 424-7.
4. Chao-Gan, Y. and Z. Yu-Feng, DPARSF: A MATLAB Toolbox for "Pipeline" Data Analysis of Resting-State fMRI. Front Syst Neurosci, 2010. 4: p. 13.
5. Tzourio-Mazoyer, N., et al., Automated anatomical labeling of activations in SPM using a macroscopic anatomical parcellation of the MNI MRI single-subject brain. Neuroimage, 2002. 15(1): p. 273-89.
6. Cha, Y.H., D. Gleghorn, and B. Doudican, Occipital and Cerebellar Theta Burst Stimulation for Mal De Debarquement Syndrome. Otol Neurotol, 2019. 40(9): p. e928-e937.
Figures
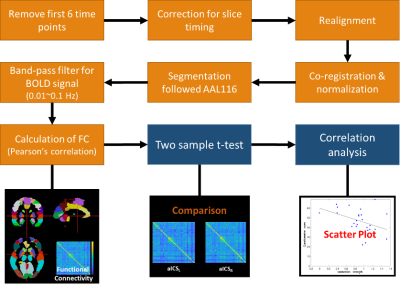
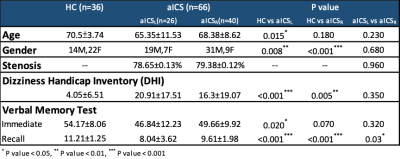
Table 1 The demography and neuropsychological assessments of study groups.