4241
Assessment of Synovitis in Osteoarthritis Using Non-Contrast Quantitative DESS1Department of Radiology, Stanford University, Stanford, CA, United States, 2Department of Radiology, University of Cambridge, Cambridge, United Kingdom, 3Norwich Medical School, University of East Anglia, Norwich, United Kingdom, 4Department of Radiology, Norfolk and Norwich University Hospital, Norwich, United Kingdom, 5Department of Mechanical Engineering, University of Saskatchewan, Saskatoon, SK, Canada
Synopsis
Quantitative double-echo in steady-state (qDESS) MRI has been proposed as an alternative to T1-weighted contrast enhanced MRI (CE-MRI) for evaluation of synovitis. In comparison with CE-MRI by, four radiologists, qDESS with a low diffusion gradient (qDESSLow), and qDESS with a high diffusion gradient (qDESSHigh) both showed good agreement to CE-MRI for the overall and regional impressions of synovitis, as well as good inter- and intra- rater agreement. Further, radiologists rated qDESSLow and qDESSHigh with moderate-to-high and moderate diagnostic confidence, respectively. This work shows the potential of the qDESS sequence as a non-contrast imaging technique for evaluation of synovitis.
Introduction
Osteoarthritis (OA) is a painful disease of the joint that affects an estimated 30 million adults in the United States1. Synovitis, or inflammation of the synovial membrane lining the joint, is an important component of osteoarthritis and is thought to play a key role in disease progression. Synovitis is typically evaluated using T1-weighted contrast-enhanced MRI (CE-MRI) following intravenous injection of a gadolinium-based contrast agent (GBCA). However, this technique is not widely utilized in clinical imaging due to increased time, complexity, cost, and risk. The quantitative double-echo in steady-state (qDESS) sequence has previously been proposed as a non-contrast method for detection of synovitis2-4. This study aims to determine the utility of non-contrast qDESS MRI for imaging of synovitis.Methods
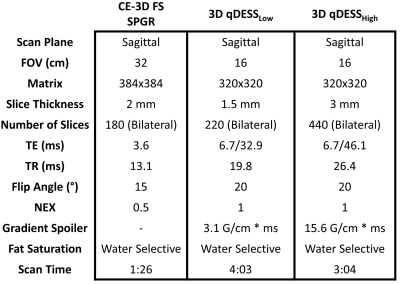
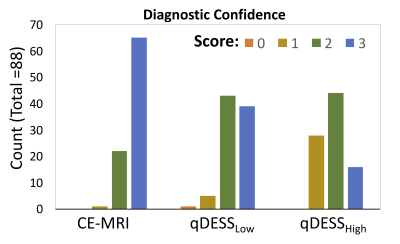
We scanned both knees of 11 patients with moderate to severe osteoarthritis and swelling in at least one knee on a 3.0 T MRI scanner (GE Healthcare). The qDESS sequence produces two echoes, the first with T2/T1 weighting and the second with higher T2-weighting and diffusion weighting, based on the spoiler gradient area. Patients were scanned using two bilateral 3D qDESS sequences: one utilizing a low diffusion gradient (2 cycles/pixel, total gradient area 3.1 (G/cm)*(ms), “qDESSLow”), and the second utilizing a high diffusion gradient (20 cycles/pixel, total gradient area 15.6 (G/cm)*(ms), “qDESSHigh”). Reference standard bilateral fat-suppressed T1-weighted CE-MR images were also acquired following intravenous injection of a GBCA (Gadovist; Bayer, Leverkusen, Germany). Additional scan parameters can be found in Table 1.Following acquisition of these sequences, the first and second qDESS echoes were combined to form hybrid fluid-nulled images according to the equation Hybrid Image = S(echo1) - β * S(echo2), where β is a weighting factor utilized to null synovial effusion2,5. qDESSHigh, qDESSLow, and CE-MR images were then randomized, blinded, and divided into three reader sets with 22 images in each. Four musculoskeletal radiologists graded images for synovitis. Readers were asked to grade an overall impression of synovitis as well as synovitis at four sites in the knee6: the suprapatellar pouch, intercondylar notch, and medial and lateral parapatellar recesses. Grading of synovitis was done on a four-point scale from 0 to 3, where 0 indicated no synovitis and 3 indicated severe synovitis. Readers also rated their diagnostic confidence on a scale from 0 to 3, with 0 indicating no diagnostic confidence and 3 indicating high diagnostic confidence. Following grading of the third set, readers were given a fourth set consisting of randomized images from the first and second image sets to assess intra-rater agreement.
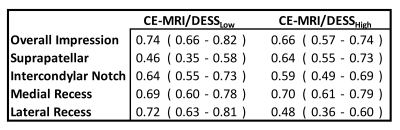
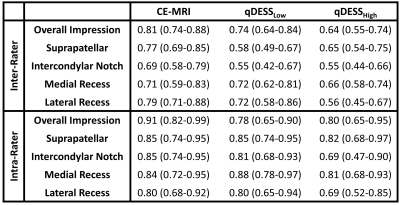
A linearly weighted Gwet's AC2 agreement coefficient was calculated to assess agreement between qDESS and CE-MRI gradings, intra-rater agreement, and inter-rater agreement7. An AC2 of <0.20 was considered poor, 0.21-0.40 was considered fair, 0.41-0.60 was considered moderate, 0.61-0.80 was considered good, and 0.81-1.00 was considered very good. Mean diagnostic confidence was also calculated.
Results
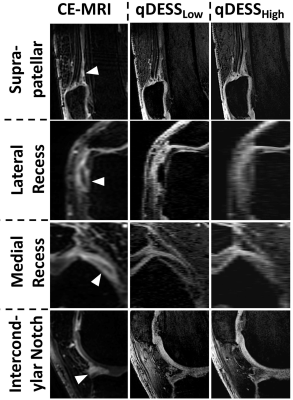
Good agreement with CE-MRI was seen for both qDESSLow (AC2=0.74) and qDESSHigh (AC2=0.66). Regional agreement between CE-MRI and qDESSLow was good at the intercondylar notch, medial recess, and lateral recess and moderate at the suprapatellar pouch, while agreement between CE-MRI and qDESSHigh was good at the suprapatellar pouch and medial recess, and moderate at the intercondylar notch and lateral recess (Table 2). Representative images of concordant radiologist gradings of synovitis between qDESS and CE-MRI are shown in Figure 1. Inter-rater agreement was very good for CE-MRI (AC2=0.81) and good for qDESSLow (AC2=0.74) and qDESSHigh (AC2=0.64) (Table 3). Intra-rater agreement was very good for CE-MRI (AC2=0.91) and good for qDESSLow (AC2=0.78) and qDESSHigh (AC2=0.80) (Table 3). Diagnostic confidence was highest for CE-MR images (mean = 2.7 ± 0.5), followed by qDESSLow (mean = 2.4 ± 0.7) and lastly qDESSHigh (mean = 1.9 ± 0.7). Distribution of diagnostic confidence gradings for each method are shown in Figure 2.Discussion
Both qDESSLow and qDESSHigh showed good agreement to reference standard CE-MRI for assessment of synovitis. In instances of disagreement between CE-MRI and qDESS, qDESS was largely seen to underestimate the degree of synovial thickening. However, this may be due to the known overestimation of synovial volume on CE-MRI due to leakage of the GBCA from the synovium into the surrounding tissue8. While diagnostic confidence for CE-MRI was highest, qDESSLow was consistently rated with moderate to high confidence, while raters tended to only have low to moderate confidence in qDESSHigh. The lower overall SNR and blurring due to increased slice thickness may have contributed to the lower agreement and diagnostic confidence seen with qDESSHigh, particularly for axial reformats, where increased slice thickness led to considerably decreased resolution.The qDESS sequence with a low diffusion gradient (qDESSLow) is already utilized both clinically and in research studies, can be used to generate accurate cartilage T2 maps9, and has shown utility as a stand-alone five-minute knee imaging protocol10. Assessment of synovitis without added scan time requirement would further increase the utility of this sequence for knee MRI as both a research and clinical tool.
In conclusion, this work shows the potential of the qDESS sequence as a non-contrast imaging technique for evaluation of synovitis. Such a method could greatly enhance clinical and research evaluation of synovitis in OA.
Acknowledgements
This work was funded by grant support from GE Healthcare and NIH grants R01-EB002524-14, R01-AR077604, R24-AR062068, and R00-EB022634.References
1. Osteoarthritis (OA). cdc.gov. https://www.cdc.gov/arthritis/basics/osteoarthritis.htm. Updated July 27, 2020. Accessed December 06, 2020.
2. Emily J McWalter, Bragi Sveinsson, Edwin H Oei, et al. Non-contrast Diffusion-weighted MRI for Detection of Synovitis using DESS. In: Proceedings of the 22nd International Society for Magnetic Resonance in Medicine (ISMRM) Annual Meeting. 2014.
3. Oei EH, McWalter EJ, Sveinsson B, Alley MT, Hargreaves BA, Gold GE. Non-contrast diffusion weighted imaging for the assessment of knee synovitis: a comparative study against contrast-enhanced MRI. Osteoarthritis Cartilage. 2014;22:S252. doi:10.1016/j.joca.2014.02.481
4. Fan AP, Fong G, Sveinsson B, et al. Automated, non-contrast MRI for detection of synovitis using diffusion-weighted dess. Osteoarthritis Cartilage. 2015;23:A240-A241. doi:10.1016/j.joca.2015.02.447
5. Thoenen J, MacKay JW, Chaudhari A, et al. Ideal Weighting Parameter for Non-Contrast Detection of Synovitis Using Diffusion-Weighted DESS. In: Proceedings of 28th Annual Meeting of ISMRM. ; 2020.
6. Rhodes LA, Grainger AJ, Keenan A-M, Thomas C, Emery P, Conaghan PG. The validation of simple scoring methods for evaluating compartment-specific synovitis detected by MRI in knee osteoarthritis. Rheumatology. 2005;44(12):1569-1573. doi:10.1093/rheumatology/kei094
7. Gwet KL. Computing inter-rater reliability and its variance in the presence of high agreement. Br J Math Stat Psychol. 2008;61(Pt 1):29-48. doi:10.1348/000711006X126600
8. Ostergaard M, Klarlund M. Importance of timing of post-contrast MRI in rheumatoid arthritis: what happens during the first 60 minutes after IV gadolinium-DTPA? Annals of the Rheumatic Diseases. 2001;60(11):1050-1054. doi:10.1136/ard.60.11.1050
9. Eijgenraam, S.M., Chaudhari, A.S., Reijman, M. et al. Time-saving opportunities in knee osteoarthritis: T2 mapping and structural imaging of the knee using a single 5-min MRI scan. Eur Radiol 30, 2231–2240 (2020). https://doi.org/10.1007/s00330-019-06542-9
10. Chaudhari AS, Black MS, Eijgenraam S, et al. 5-Minute Knee MRI for Simultaneous Morphometry and T2 Relaxometry of Cartilage and Meniscus and for Semi-Quantitative Radiological Assessment using Double-Echo in Steady-State at 3T. J Magn Reson Imaging JMRI. 2018;47(5):1328-1341. doi:10.1002/jmri.25883
Figures