4238
Whole-body MRI reveals the burden of unsuspected synovitis in juvenile idiopathic arthritis1Centre for Medical Imaging, University College London, London, United Kingdom, 2Centre for Adolescent Rheumatology Versus Arthritis at UCL UCLH and GOSH, University College London, London, United Kingdom, 3Radiology, University College London Hospital, London, United Kingdom, 4Medical Physics, University College London Hospitals, London, United Kingdom, 5Adolescent and young adult Rheumatology, University College London Hospital, London, United Kingdom
Synopsis
MRI is used for the detection of synovitis in juvenile idiopathic arthritis (JIA). We developed a whole-body MRI protocol, consisting of coronal, post-contrast mDixon images, which is fast and offers good coverage of peripheral joints and spine. A prospective study including 32 adolescent and young adult patients with JIA revealed that 43.8% of patients had synovitis in at least one joint on imaging that was not detectable clinically. The proportion of patients with subclinical synovitis was similar in clinically active and inactive patients. This could lead to identification of unsuspected inflammation in JIA patients with potential impact on their treatment.
Introduction
Magnetic resonance imaging can facilitate the diagnosis of juvenile idiopathic arthritis (JIA), but is also increasingly used for monitoring disease activity in individual joints. We developed a whole-body MRI protocol (WBMRI) to assess synovitis in young people, which is fast and tolerable. This prospective study aims to measure the frequency of subclinical synovitis on WBMRI, in adolescent patients with JIA.Methods
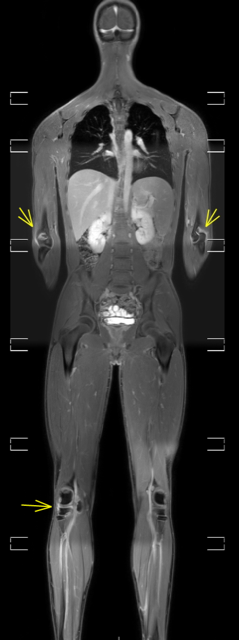
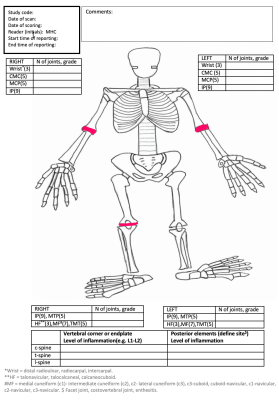
The WBMRI protocol included post-contrast mDixon images divided into seven anatomical stations. There was an additional station for ankles and feet, when not visualised due to patient’s height. The stitching of images into a single full-field coronal view was automated. Imaging parameters and body positioning were first optimised in volunteers to improve image quality and coverage of hands, elbows and feet. Subsequently, JIA patients were recruited from a tertiary adolescent and young adult rheumatology clinic, between September 2019 and August 2020. All patients were examined by a senior rheumatology trainee, before undergoing a WBMRI scan on the same day. Patients were assigned to a clinically active or inactive group, depending on their active joint count (AJC); active patients had AJC≥ 1, while the clinically inactive patients had an AJC =0. The duration of the post-contrast imaging, including the additional station, the administration of contrast and hand positioning was 15 minutes. One experienced musculoskeletal radiologist, blinded to clinical information, reviewed all the scans. The assessment of synovitis was based on post-contrast, water-only mDixon images, performed in a 3 Tesla scanner (Figure 1 and 2). Only joints that were definitely abnormal were counted as synovitic (Figure 3). Eighty-one joints per patient were examined clinically and with imaging. The presence of subclinical synovitis in a patient was defined as synovitis in one or more joints on MRI, which were not active clinically.Results
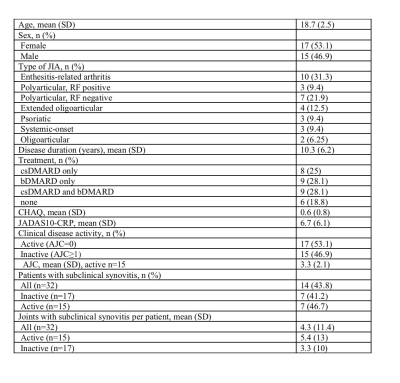
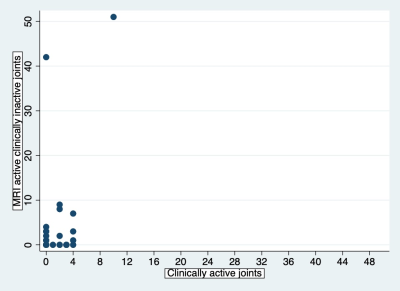
Thirty-two patients aged 15 to 24 were included in the analysis. The patient characteristics and the frequency of subclinical synovitis are summarised in Table 1. Subclinical synovitis was detected in a similar proportion of JIA patients in both active and inactive groups (46.7% vs. 41.2%, P =0.76). The relationship between clinically active joints and subclinical synovitis is depicted in Figure 4. The most frequent region with subclinical synovitis was the hindfoot, detected in 22% (7/32) of JIA patients and 17.2% (11/64) of hindfoot joints assessed by MRI. The second most common joint with clinically unsuspected inflammation was the knee, found in 19% (6/32) of JIA patients and 14% (9/64) of knee joints. Similarly, 16% (5/32) of the adolescent patients had active disease in the hip, ankle or midfoot joints. The frequency of elbow involvement was also considerable, with 12% (7/58) of joints with subclinical synovitis in 14% (4/29) of JIA patients.Conclusion
In conclusion, we describe a protocol for performing WBMRI in young patients with JIA, relying on post-contrast mDixon images. This protocol reveals a large burden of clinically undetected synovitis in both clinically active and clinically inactive groups. This could help to identify and enable the treatment of inflammation earlier in patients' disease course.Acknowledgements
This study was supported by the British Society of Rheumatology [179978 to VC] and Action Medical Research [GN2697 to MHC]. The author would like to thank both for their help and support.
Dr Timothy P.J. Bray is funded by the National Institute for Health Research (NIHR).
Professor Margaret Hall-Craggs is supported by the University College London Hospitals Biomedical Research Centre (UCLH BRC).
References
No reference found.Figures