4233
Assessment of Osteoporosis in Human Lumbar Using 3D Adiabatic Inversion Recovery Prepared Ultrashort TE Cones Sequence1Department of Radiology, The Fifth Affiliated Hospital of Sun Yat-Sen University, Zhuhai, China, 2Department of Radiology, University of California, San Diego, CA, United States, 3MR Research, GE Healthcare, Guangzhou, China
Synopsis
The 3D adiabatic inversion recovery prepared ultrashort TE cones (3D IR-UTE) sequence can image and quantify proton density assessment of short T2 water components in trabecular bone in vivo, and has the potential to diagnosis people with osteoporosis. The current study aims to prospective investigate the performance in diagnosing osteoporosis of IR-UTE sequence in human lumbar and to compare with quantitative computed tomography (QCT), dual-energy X-ray absorptiometry (DXA) and Fracture Risk Assessment Tool (FRAX) scores. It was concluded that IR-UTE was positively correlated to QCT and DXA, and was negatively correlated to FRAX scores.
Introduction
Osteoporosis (OP) is a systemic metabolic disease characterized by decreased bone strength and increased risk of fracture due to low bone mass and microarchitectural deterioration of bone tissue.[1] Many studies have reported a strong correlation of bone mineral density (BMD) with osteoporosis.[2] In this study, we assess the performance of broadband adiabatic inversion recovery prepared 3D UTE Cones (3D IR-UTE) sequence[3] in the diagnosis of patients with osteoporosis in lumbar, and comparing performance against the current quantitative computed tomography (QCT), dual-energy X-ray absorptiometry (DXA) and Fracture Risk Assessment Tool (FRAX) reference standard.Methods
30 osteoporosis patients (age 56 ± 16 years, age range 40-79 years) were recruited and underwent 3D IR-UTE sequence to imaging lumbar on a 3.0T MRI scanner (Signa, Pioneer, GE Healthcare). A MnCl4 doped water phantom with a T2* around 0.34 ms was placed between the patients and the spine coil during scanning to serve as a reference to calibrate the proton density (PD) of trabecular bone.[3] The IR-UTE sequence parameters were as follows: TR/TI = 150/64 ms, TE = 0.032 ms, flip angle = 18°, FOV = 30cm × 30cm, matrix = 140 × 140, slice thickness = 4.5mm, slice number = 16, oversampling factor = 2, and scan time = 10 min. QCT examinations of the lumbar region in the supine position were performed on a 128-channel multi-detector CT scanners (uCT 760, United Imaging Healthcare). The QCT images were acquired using the following parameters: collimation = 0.625 mm; tube voltage = 120 kVp; tube current, automatic. DXA scanning (Osteocore, Medilink) was performed by using standard methods to compute BMD T scores in the lumbar. For the QCT and DXA BMD of spinal trabecular bone, a QCT value greater than 120 mg/cm3 (equivalent to a DXA T-score of –1.0 SD) is considered normal, a QCT value between 80 mg/cm3 and 120 mg/cm3 indicates osteopenia, and QCT BMD less than 80 mg/cm3 (equivalent to a DXA T-score of –2.5SD) indicates osteoporosis.[4] Square regions of interest (ROIs) were placed in the vertebral body, cortical bone were avoided. We measured the intravertebral PD and BMD in L2-L4. Pearson correlation analysis was performed to calculate the correlations between PD measured by IR-UTE and BMD measured by QCT, DXA, respectively, in all patients. Mean lumbar PD was computed for each subject by averaging the PD measurements from three vertebrae (L2–L4) and Pearson correlation analysis was performed to calculate the correlations between mean lumbar PD and FRAX scores. Receiver operating characteristic (ROC) analyses were applied to assess the diagnostic utility of IR-UTEQCT (taking QCT as gold standard for diagnosis) and IR-UTEDXA (taking DXA as gold standard for diagnosis) in the differentiation between healthy and osteopenic subjects, between healthy and osteoporotic subjects, as well as between osteopenic and osteoporotic subjects. A value of P < 0.05 was considered as a statistically significant.Results
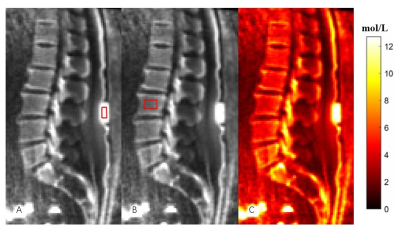
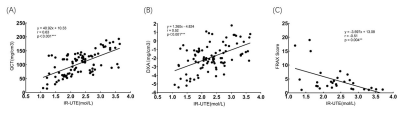
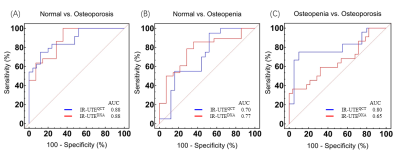
Figure 1 shows the representative lumbar IR-UTE images acquired from a 56-year-old female osteoporosis volunteer. The vertebral PD measured by IR-UTE showed a strong positive correlation with BMD measured by QCT (r = 0.632, P < 0.001) (Fig. 2A) and BMD measured by DXA (r = 0.517, P < 0.001) (Fig. 2B), and showed a negative correlation with FRAX score (r = -0.515, P = 0.004) (Fig. 2C). These results demonstrated that the vertebral PD increased with BMD. The ROC curves of IR-UTEQCT and IR-UTEDXA demonstrated good performance in differentiating normal vs. osteoporosis (AUC of IR-UTEQCT = 0.88, AUC of IR-UTEDXA = 0.88) (Fig. 3A), normal vs. osteopenia (AUC of IR-UTEQCT = 0.70, AUC of IR-UTEDXA = 0.77) (Fig. 3B), and osteopenia vs. osteoporosis (AUC of IR-UTEQCT = 0.80, AUC of IR-UTEDXA = 0.65) (Fig. 3C).Discussion and Conclusion
In this prospective study, we introduced a novel quantitative MRI for lumbar spine bound water imaging, i.e. IR-UTE measured PD, using lumbar QCT and DXA as a reference standard for identifying patients at increased risk of osteoporosis. We found that measured bound water PD has a very good correlation with BMD during the development of osteoporosis in human lumbar. The 3D IR-UTE measures demonstrated good performance in the differentiation of normal, osteopenia and osteoporosis. The IR-UTE measured PD may be a promising marker for assessing patient with osteoporosis.Acknowledgements
No acknowledgement found.References
[1] A H. Osteoporosis prevention, diagnosis, and therapy. Jama 2001;285(6):785-795.
[2] Li N, Li XM, Xu L, Sun WJ, Cheng XG, Tian W. Comparison of QCT and DXA: Osteoporosis Detection Rates in Postmenopausal Women. International journal of endocrinology 2013;2013:895474.
[3] Ma YJ, Chen Y, Li L, Cai Z, Wei Z, Jerban S, Jang H, Chang EY, Du J. Trabecular bone imaging using a 3D adiabatic inversion recovery prepared ultrashort TE Cones sequence at 3T. Magnetic resonance in medicine 2020;83(5):1640-1651.
[4] Engelke K, Adams JE, Armbrecht G, Augat P, Bogado CE, Bouxsein ML, Felsenberg D, Ito M, Prevrhal S, Hans DB, Lewiecki EM. Clinical use of quantitative computed tomography and peripheral quantitative computed tomography in the management of osteoporosis in adults: the 2007 ISCD Official Positions. Journal of clinical densitometry : the official journal of the International Society for Clinical Densitometry 2008;11(1):123-162.
Figures