4231
Evaluation of Lumbar Disc Herniation Using Ultrashort Echo Time Magnetization Transfer in Posterior Longitudinal Ligament and Nucleus Pulposus1Department of Radiology, The Fifth Affiliated Hospital of Sun Yat-Sen University, Zhuhai, China, 2Department of Radiology, University of California, San Diego, CA, United States, 3MR Research, GE Healthcare, Guangzhou, China
Synopsis
Magnetization transfer ratio (MTR) has been used for assessment of macromolecules in biological tissues. Ultrashort echo time technique magnetization transfer (UTE-MT) can quantify both of short and long T2 tissues, may have potential to evaluate early disc herniation. The current study aims to assess the feasibility of UTE-MT quantification of posterior longitudinal ligament and nucleus pulposus for evaluation of early disc herniation. It was concluded that the UTE-MT sequence is feasible to quantify posterior longitudinal ligament and nucleus pulposus in lumbar. Posterior longitudinal ligament and nucleus pulposus UTE-MTR may provide a new opportunity for early prediction of lumbar disc herniation.
Introduction
Lumbar discectomy is the most common surgical procedure for patients with back pain in the United States, with over 300,000 discectomy procedures every year.[1]The degeneration or ossification of posterior longitudinal ligament and nucleus pulposus may be closely related to the early disc herniation. However, the T2 of the posterior longitudinal ligament is relatively short and cannot be effectively imaged in conventional clinical sequences. Ultrashort echo time magnetization transfer (UTE-MT) sequence with TEs less than 100 μs can be used for imaging and quantifying both short and long T2 tissues. The derived index magnetization transfer ratio (MTR) [2] may be potentially useful for early disc herniation assessment. In this study, we utilized UTE-MT sequence to investigate the correlations between UTE-MTR of posterior longitudinal ligament/nucleus pulposus and lumbar disc herniation.Methods
A total of 50 disc herniation patients (age 47 ± 16 years, age range 34-75 years) were recruited and underwent UTE-MT sequence of lumbar on a 3.0T MRI scanner (Signa, Pioneer, GE Healthcare). A Fermi pulse was employed to generate the MT contrast in UTE-MT sequence with duration of 8ms and bandwidth of 160Hz. The frequency offset of this MT pulse was 1500 Hz. The UTE-MT sequence was scanned twice with flip angle of 750° for MT-On and 0° for MT-Off. Other UTE-MT sequence parameters were as follows: TR = 100 ms, TE = 0.032 ms, excitation flip angle = 5°, number of spokes per-TR = 5, FOV = 28cm × 28cm, matrix = 140 × 140, slice thickness = 3.6mm, and slice number = 16, oversampling factor = 1.2, and scan time = 3min. The ROI of the posterior longitudinal ligament and nucleus pulposus was manually delineated by a radiologist with 10 years of experience. The grade of disc herniation was divided into disc herniation and non disc herniation by a radiologist with 15 years of experience. Then, according to Michigan State University (MSU) classification of lumbar disc herniation[3], lumbar disc herniation was divided into grade 1, grade 2 and grade 3, and no herniated disc was defined as grade 0. Pearson correlation analysis was performed to calculate the correlations between posterior longitudinal ligament/nucleus pulposus UTE-MTR value and two kinds of classification of disc herniation. A one way ANOVA test was used to compare posterior longitudinal ligament and nucleus pulposus UTE-MTR between different grades of disc herniation. A value of P < 0.05 was considered as a statistically significant.Results
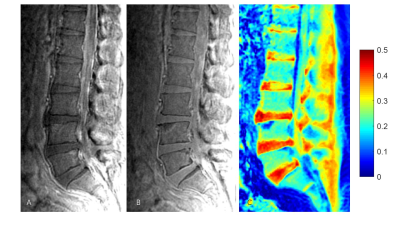
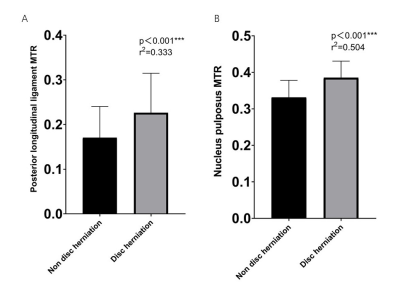
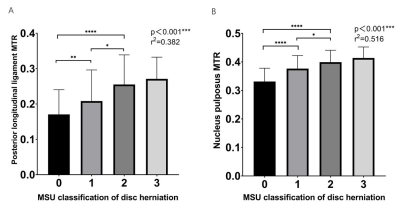
Figure 1 shows the representative lumbar UTE-MT images acquired from a 63-year-old male disc herniation volunteer. The posterior longitudinal ligament and nucleus pulposus UTE-MTR showed a positive correlation with disc herniation (r2= 0.333, P < 0.001; r2= 0.504, P < 0.001, respectively) (Figure 2). The posterior longitudinal ligament and nucleus pulposus UTE-MTR showed a positive correlation with MSU classification of disc herniation (r2= 0.382, P < 0.001; r2= 0.516, P < 0.001, respectively) (Figure 3).Discussion and Conclusion
To our best knowledge, this is the first prospective study of applying UTE-MT in posterior longitudinal ligament and nucleus pulposus to assess lumbar disc herniation. Our findings suggested that the high UTE-MTR of posterior longitudinal ligament and nucleus pulposus associate with more severe lumbar disc herniation in patients. In conclusion, the UTE-MTR of posterior longitudinal ligament and nucleus pulposus may be a promising biomarker to predict early disc herniation in lumbar spine.Acknowledgements
No acknowledgement found.References
[1] Atlas SJ, Deyo RA, Patrick DL, Convery K, Keller RB, Singer DE. The Quebec Task Force classification for Spinal Disorders and the severity, treatment, and outcomes of sciatica and lumbar spinal stenosis. Spine (Phila Pa 1976) 1996;21(24):2885-2892.
[2] Ma YJ, Chang EY, Carl M, Du J. Quantitative magnetization transfer ultrashort echo time imaging using a time-efficient 3D multispoke Cones sequence. Magnetic resonance in medicine 2018;79(2):692-700.
[3] Mysliwiec LW, Cholewicki J, Winkelpleck MD, Eis GP. MSU classification for herniated lumbar discs on MRI: toward developing objective criteria for surgical selection. European spine journal : official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society 2010;19(7):1087-1093.
Figures