4170
Clinical Evaluation of Isotropic MAVRIC-SL at 3T1Stanford University, Stanford, CA, United States
Synopsis
For the past decade, the development of 3D multispectral imaging (MSI) approach has facilitated the early detection of complications around metallic implants. However, the long acquisition time and need for multi-planar acquisitions make it difficult for symptomatic, elderly patients to tolerate. In this preliminary study, we evaluate the use of a fast isotropic 3D MSI technique at 3T MRI, which can potentially replace multiple sequences of orthogonal imaging planes with a single acquisition. Our results show promise for the improved visualization of various hardware complications using image reformats on arbitrary planes with diagnostically acceptable image quality.
Introduction
3D multispectral imaging (MSI) approaches (1-3) have been widely used during the last decade to evaluate complications occurring near metallic implants following total joint arthroplasties. The technique employs 3D acquisitions for a number of spectral bins to mitigate severe signal loss artifacts around metal that conventional sequences suffer from. However, repeated 3D acquisitions of 3D MSI and the need of multiplanar acquisitions for optimal visualization of different pathologies (4,5) can make the overall scan time difficult to tolerate for patients in pain. An isotropic 3D MSI approach, if the scan time is clinically acceptable, may alleviate the need for multiplanar acquisitions by allowing image reformats on the arbitrary plane of choice. For 1.5T MRI, such an isotropic 3D MSI acquisition recently became feasible by the scan time acceleration with spectral calibration (6). In this study, we implemented an isotropic 3D MSI approach for 3T MRI with a novel compressed sensing algorithm based on robust PCA (7) and present the pilot evaluation result from 15 total hip replacement patients with 22 total hip replacements.Methods
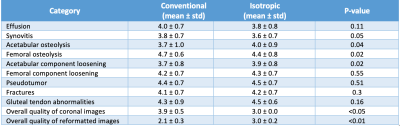
All subjects in our study signed a written consent form approved by our institutional review board for participation in the study. 15 symptomatic patients with 22 total hip implants were recruited, and all scans were conducted on 3T GE MRI scanners (Discovery MR 750, GE Healthcare, Waukesha, U.S.) with a 32-channel body coil array for signal reception. The imaging protocol included a conventional coronal MAVRIC-SL sequence and the proposed isotropic MAVRIC-SL sequence acquired in the coronal plane for 3D MSI acquisitions. The pulse sequence parameters for conventional MAVRIC-SL/isotropic MAVRIC-SL were as follows: TR = 4/3.2sec TE = 6.4/6.1ms, ETL = 20/28, FOV = 48x48/48x48cm, Matrix = 384x256/256x256, Slice thickness = 4/1.6mm, Bandwidth = ±125/±125KHz, Undersampling factor (phase x slice) = 2x2/4x4. Both sequences used partial Fourier sampling for additional undersampling.Two musculoskeletal radiologists reviewed the images from conventional and isotropic MAVRIC-SL. The conventional MAVRIC-SL images were interpolated to the same slice thickness (1.6mm) before review to avoid sequence recognition by the slice thickness. Images were scored on the presence/absence of different pathologies (effusion, synovitis, acetabular osteolysis, femoral osteolysis, pseudotumor, fractures, and gluteal tendon abnormalities), with degree of confidence using a 5-point scale (1: low, 5: high). The overall quality of the coronal images and images reformatted on axial and sagittal planes was also scored on a 5-point scale (1: poor, 5: excellent). The resulting scores were compared using the Wilcoxon signed rank test. Other sequences in the exam protocol and available patient clinical records were employed later for confirming pathology identified on the study sequences.
Results
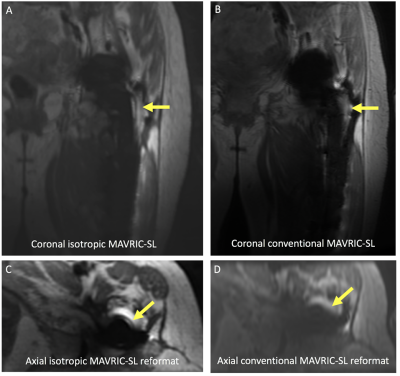
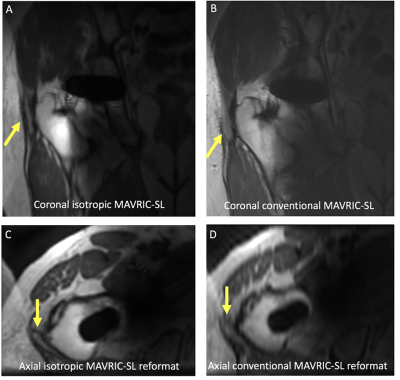
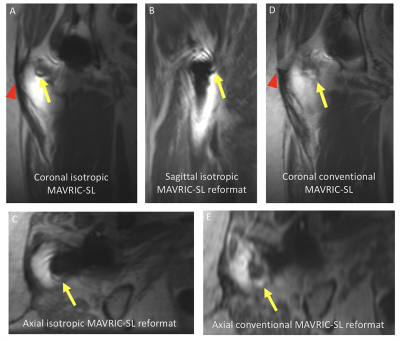
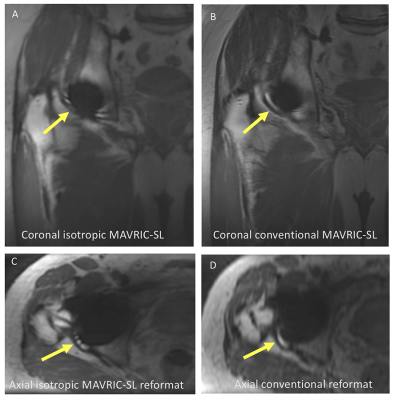
The average scan time was 6 minute and 58 seconds for the conventional MAVRIC-SL and 4 minute and 10 seconds for the isotropic MAVRIC-SL. Overall, the difference of confidence between isotropic MAVRIC-SL was not significant (p < 0.05) in most cases, as shown in Figure 1, except for the detection of acetabular osteolysis, acetabular component loosening (more confident with isotropic MAVRIC-SL) and femoral osteolysis (more confident with conventional MAVRIC-SL). While image quality of the isotropic sequence was lower than the conventional sequence in the original coronal-acquisition plane (p<0.05), the reformatted image quality was higher for isotropic MAVRIC-SL sequence than conventional MAVRIC-SL (p < 0.01). The axial and sagittal reformats either changed the diagnosis or increased diagnostic confidence in 14% of reviews for conventional imaging, compared to 64% of reviews for isotropic imaging.There were 7 cases where the presence of potential pathologies was different between the two sequences, and isotropic MAVRIC-SL resulted in better detection of an abnormality or higher diagnostic confidence than conventional MAVRIC-SL (5 vs 2 cases). The 5 cases in which isotropic imaging had improved detection included pseudotumor (2), femoral loosening (1), femoral osteolysis (1) and a small effusion (1). Examples are shown in Figures 2 - 4. The cases in which conventional imaging had more accurate detection included a small effusion (1) ( Figure 5), and gluteal tendon tearing (1).
Discussion
The proposed isotropic MAVRIC-SL approach achieved a comparable degree of diagnostic confidence for most types of pathology evaluated. The increased confidence of isotropic MAVRIC-SL was achieved when assessment of reformatted images revealed abnormalities that were obscured or not as well seen on the coronal acquisition plane, as evidenced by the large number of cases in which isotropic reformats either changed the radiologists’ diagnosis or increased their diagnostic confidence. The lower scores for image quality and decrease of confidence for isotropic imaging in certain cases compared to conventional imaging is likely to stem from a few factors including reconstruction artifacts from aggressively undersampled data, blurring from longer echo train length and lower resolution in the frequency encoding direction. We believe these issues can be addressed by relaxing the undersampling rate and tuning the sequence parameters without causing significant increase of scan time.Conclusion
We conducted a pilot study on a fast isotropic 3D MSI technique compared to conventional MAVRIC-SL imaging at 3T. The availability of better quality multiplanar reconstructions demonstrated promise for improving the radiologist’s diagnostic confidence and potentially diagnostic accuracy.Acknowledgements
This work was supported by NIH R56AR077706 and GE Healthcare.References
1. Lu W, Pauly KB, Gold GE, Pauly JM, & Hargreaves BA (2009) SEMAC: Slice Encoding for Metal Artifact Correction in MRI. Magn Reson Med 62(1):66-76.
2. Koch KM, Lorbiecki JE, Hinks RS, & King KF (2009) A multispectral three-dimensional acquisition technique for imaging near metal implants. Magn Reson Med 61(2):381-390.3.
3. Koch KM, et al. (2011) Imaging near metal with a MAVRIC-SEMAC hybrid. Magn Reson Med 65(1):71-82.4.
4. Fritz J, Lurie B, Miller TT, & Potter HG (2014) MR imaging of hip arthroplasty implants. Radiographics 34(4):E106-132.5.
5. Fritz J, Lurie B, & Potter HG (2015) MR Imaging of Knee Arthroplasty Implants. Radiographics 35(5):1483-1501.6.
6. Zochowski KC, et al. (2019) MRI of Hip Arthroplasties: Comparison of Isotropic Multiacquisition Variable-Resonance Image Combination Selective (MAVRIC SL) Acquisitions With a Conventional MAVRIC SL Acquisition. AJR Am J Roentgenol 213(6):W277-W286.
7. Levine E, Stevens K, Beaulieu C, & Hargreaves B (2018) Accelerated three-dimensional multispectral MRI with robust principal component analysis for separation of on- and off-resonance signals. Magn Reson Med 79(3):1495-1505.
Figures