4162
The Impact of Acceleration Factors of Compressed Sensing on the Image Quality of 3D-TOF-MRA for Cervical Vessels1Department of Radiology, the First Affiliated Hospital of Dalian Medical University, Dalian, China, 2PHILIPS——Philips Healthcare, beijing, China
Synopsis
Traditional 3D-TOF Magnetic Resonance Angiography (MRA) in carotid imaging needs a relatively long scan time and is prone to be disturbed by motion artifacts such as vascular pulsation, respiratory movement, and some other physiological factors. A combination of compressed sensing (CS) can achieve high acceleration factors and thus lead to a significant reduction of scan time. Here, we investigated the impact of acceleration factors of compressed sensing on the image quality of 3D-TOF-MRA for cervical vessels. CS acceleration factor of 6 is recommended for clinical 3D-TOF carotid MRA to achieve an optimal balance between imaging time and image quality.
Introduction
3D-TOF magnetic resonance angiography (MRA)1 enables non-invasive visualization of the anatomical structure of blood vessels. It has been widely used for the measurement of vascular morphology and detection of carotid artery stenosis 2. However, the traditional 3D-TOF MRA often needs a relatively long scan time, during which the patient's swallowing, respiratory movement, neck movement, etc. might result in motion artifacts and thus hamper the follow-up diagnosis3. For patients with carotid artery stenosis, it is difficult to maintain a long time immobile state due to cerebral hemodynamic insufficiency. The CS technique 4 was proven a powerful tool for MR imaging acceleration 5-6. The purpose of this study was to explore the impact of acceleration factors of CS on the image quality of 3D-TOF-MRA for cervical vessels and to find an optimal acceleration factor to reduce the scan time without degeneration of image quality.Materials and methods
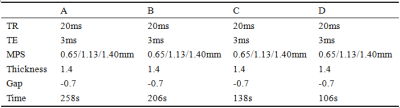
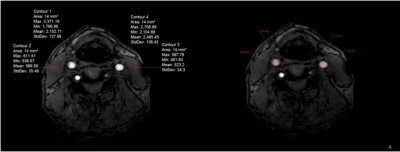
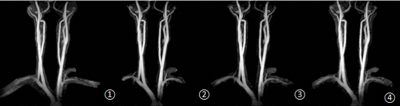
22 healthy volunteers (15 males, 54.41±18.18 years) were recruited and underwent the 3D-TOF MRA scan of neck vessels on a 3.0 T MR scanner (Ingenia CX, Philips Healthcare, Best, the Netherlands). Four groups with different acceleration schemes were set up in our study, group A with a routine clinical setup of SENSE acceleration factor 3, and groups B, C, and D with CS factors of 4, 6, and 8. The scan time for the 4 groups were 258s, 206s, 138s, and 106 s, respectively. Other scan parameters were shown in Table 1. Regions of interest were placed manually at both sides of the carotid artery and nearby sternocleidomastoid muscle by experienced radiologists for measurement of signal intensity, standard deviation, and diameter of carotid artery vessels (Figure 1). Signal to Noise Ratio (SNR) and Contrast to Noise Ratio (CNR) were calculated from the labeled ROIs for all volunteers. The two observers used a four-point scoring method to evaluate the quality of the four groups of images: 3, excellent (high quality, high intensity of arterial vessels, clear contour, no artifacts, and clear display of primary and secondary branch vessels); 2, good (strong signal of arterial vessels, clear contour, and clear first-grade branch vessels); 1, fair (strong signal of the artery, moderately clear contour, and unclear branch of the artery, with a few artifacts which did not hamper the diagnosis); 0, poor (shallow arterial angiography, unclear contour which can not meet the diagnostic requirements). The SNR and CNR on the left and right sides of the carotid artery and nearby sternocleidomastoid muscle were compared with a Wilcoxon-rank sum test. The Kappa statistics were calculated for determining the interobserver agreement. The assessment of intermethod agreement was based on the evaluation of the senior physicians. Kruskal-Wallis test was employed to assess the difference of SNR, CNR, the largest, smallest diameters of the common carotid arteries and image scores between the 4 groups. Mann-Whitney U test was used to make a pairwise comparison. This study has been approved by the local IRB.Results
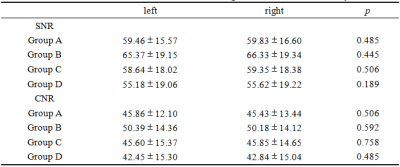
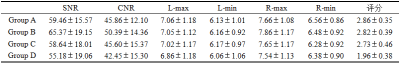
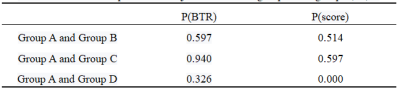
SNR and CNR from two sides of the carotid artery are in good agreement (Table. 2). Scores measured by two observers are in good agreement (p=0.880). There were no statistically significant differences in SNR, CNR, the largest and smallest diameters of the common carotid arteries between the four groups. However, if CS acceleration factor of 8 was used, the subjective scores decreased obviously (p < 0.05, Table. 3). And no significant differences of image quality were detected between conventional SENSE acceleration with a factor of 3 and CS acceleration with factors of 4 and 6.Discussion and Conclusions
Scan time for the cervical vascular 3D-TOF MRA could be reduced significantly by CS technique. However, if a large CS acceleration factor (≥ 8) is used, the image quality degrades evidently. CS acceleration factor of 6 is recommended for clinical 3D-TOF carotid MRA to achieve an optimal balance between imaging time and image quality.Acknowledgements
No acknowledgement found.References
1. Haifeng Liu, Yongsheng Xu, Yangqin Xun, et al. Diagnostic value of 3D time-of-flight magnetic resonance angiography for detecting intracranial aneurysm: a meta-analysis. Neuroradiology. 2017;59(11):1083-1092.
2. Yamada K, Yoshimura S, Shirakawa M, et al. High intensity signal in the plaque on routine 3D-TOF MRA is associated with ischemic stroke in the patients with low-grade carotid stenosis. Neurol Sci. 2018;385:164-167.
3. Bo Li, Hao Li, Li Dong, Guofu Huang, Fast carotid artery MR angiography with compressed sensing based three-dimensional time-of-fight sequence. Magn Reson Imaging. 2017;43:129-135.
4. Bratke G, et al. Accelerated MRI of the lumbar spine using compressed sensing: quality and efficiency. Magn Reson Imaging. 2018;49: 164-175.
5. Seung Hyun Leea, Young Han Lee, Jin-Suck Suh. Accelerating knee MR imaging: Compressed sensing in isotropic three-dimensional fast spin-echo sequence. Magn Reson Imaging. 2018;46:90-97.
6. Alessandro Furlana, Ersin Bayram, Senthur Thangasamy, Dale Barleya, Anil Dasyam. Application of compressed sensing to 3D magnetic resonance cholangiopancreatography for the evaluation of pancreatic cystic lesions. Magn Reson Imaging. 2018;52:131-136.
Figures