4145
High-Resolution Vessel Wall Imaging: Association of Plaque with Morphological Changes of Lenticulostriate Arteries in SSIs1Radiology, Tianjin Huanhu Hospital, Tianjin, China, 2MR Collaboration, Siemens Healthcare Lid., Beijing, China, 3Radiology, Tongde Hospital of Zhejiang Province, Hangzhou, China, 4State Key Laboratory of Brain and Cognitive Science, Institute of Biophysics, Chinese Academy of Sciences, Beijing, China
Synopsis
This study evaluated the association between plaque existence and lenticulostriate artery (LSA) morphology using high-resolution vessel wall imaging (HR-VWI) in patients with lenticulostriate infarction and non-stenotic middle cerebral artery (MCA). Patients were divided into plaque and non-plaque groups based on the plaque presence in the MCA-M1 segment of the infarcted hemisphere. Atheromatous plaque was found in 52.8% of patients, and the laterality index of the LSA and total length were higher in the plaque group. These findings suggest that HR-VWI may help distinguish branch from non-branch atheromatous small vessel disease.
Introduction
In single subcortical infarctions (SSIs) of lenticulostriate arteries (LSA) with non-stenotic middle cerebral artery (MCA), differentiating the two main pathogeneses is difficult for various reasons: 1) branch atheromatous disease (BAD), an occlusion or stenosis at a deep penetrating artery orifice, due to the presence of atheromatous plaque, and 2) lipohyalinosis and fibrinoid degeneration in small vessel disease (SVD), mainly due to the lack of in vivo imaging technique to directly visualize the MCA plaques and the LSA orifice [1]. High-resolution vessel wall imaging (HR-VWI) is capable of imaging both large-vessel wall and the LSA lumen simultaneously in one imaging setting [2], This permits further exploration of the pathogenesis of SSIs. This study aimed to investigate the association between plaque existence and LSA morphological changes using HR-VWI.Methods
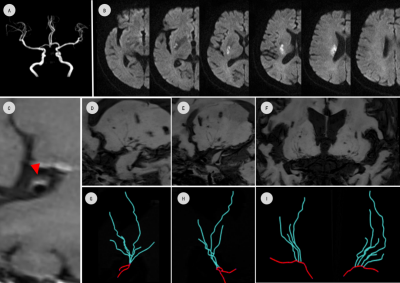
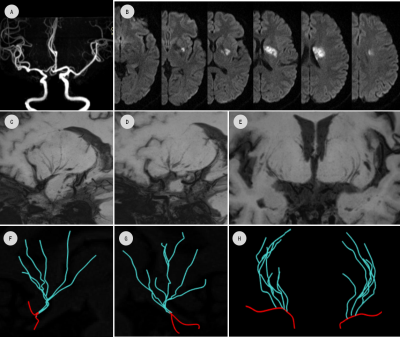
Fifty-three patients (age: 49.6±12.8 years) with acute lenticulostriate infarction and without MCA stenosis on magnetic resonance angiography (MRA) were imaged. All patients received conventional diffusion-weighted imaging (DWI), 3D time-of-flight MRA, and HR-VWI on a 3T system (MAGNETOM Skyra, Siemens Healthcare, Erlangen, Germany) with a 20-channel head-neck coil. HR-VWI was performed using the SPACE (Sampling Perfection with Application-optimized Contrast using different flip angle Evolutions) sequence with parameters: sagittal orientation,FOV=230×230 mm2,slices =240, voxel size=0.53×0.53×0.53 mm3, TR /TE =900ms/15ms, echo train length=52,scan time=8min7s.Lesion characteristics were independently assessed on DWI by two neuroradiologists, including infarct length and location (proximal or not), total cerebral small vessel disease (CSVD) score, and the MCA-M1 plaque location. MCA and LSA centerlines were traced using Sim Vascular software (http://simvascular.github.io/) to build the vascular skeleton. LSA skeletons were examined by a third senior radiologist to ensure accuracy. Representative HR-VWI images and LSA tracing results from two patients are shown in Figures 1 and 2.
LSA morphological parameters including numbers of stems and branches as well as total length on infarcted and healthy sides were recorded for each patient. Finally, laterality index (L_index) of LSA stem number, branch number, and total length were derived and defined as: L_Index = (Datainfarcted side - Datahealthy side)/(Datainfarcted side + Datahealthy side). Categorical variables were assessed using Fisher's exact test or χ2 test. Normally distributed continuous variables were analyzed by independent or paired-sample t-tests, while nonnormal variables were analyzed by the Mann-Whitney U-test.
Results
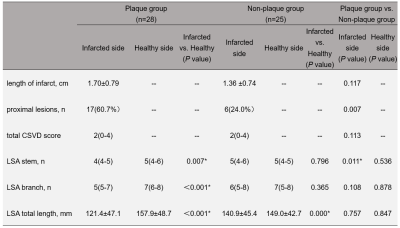
Plaques were detected on the MCA-M1 segment in the infarcted side of 28 (52.8%) patients, making up the ‘plaque’ group; the 25 patients were classified into the ‘non-plaque’ group.Table 1 summarizes infarct lesion characteristics, total CSVD score, and direct LSA morphological parameters between groups and hemispheres. Infarct length was larger in plaque versus non-plaque group (1.70 ±0.79 vs. 1.36 ±0.74 cm), but the difference was not statistically significant (P=0.117). Plaque group proximal lesion incidence was higher (P=0.007). Total CSVD score was not significantly different between two groups (P=0.113).
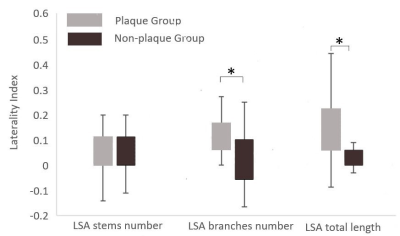
For LSA morphological parameters, plaque group LSA stems, branches, and total length in the infarcted side were lower than those in the healthy side. However, in the non-plaque group, only infarcted side LSA total length was shorter than that of the healthy side. Between groups, the LSA stems of infarcted side in the plaque group were less than that in the non-plaque group. Finally, LSA branch L_index (P=0.005) and total length (P = 0.002) in the plaque group were higher than those in the non-plaque group (Figure 3).
Discussion & Conclusion
Here we present comprehensive investigation of MCA-M1 segment plaque prevalence and its association with LSA morphological change in SSI with non-stenotic MCA.Over half of patients had plaques, implying that large artery atherosclerotic plaques occluding the LSA orifices, termed BAD, are an important cause of SSIs [3]. Furthermore, the infarcted side had fewer LSA stems and branches and lower total length than the healthy side in the plaque group, but only shorter total length was found in the non-plaque group. This supports the concept that proximal plaque occlusion of LSAs causes blood flow disturbance of the microvessel, leading to decreasing imaging signal intensity and undetectable LSAs.
Most notably, we found that the L_index of LSA branches and total length in the plaque group were higher than those in the non-plaque group, while no significant difference was found in the number of LSA branches and total length between these two groups. L_index is a derived parameter representing the LSA morphological difference between the infarcted and healthy sides, which could reduce the impact of individual differences in LSA morphology. Our findings indicate that L_index may be a candidate biomarker to identify BAD in SSIs.
In conclusion, HR-VWI was an effective method to detect plaques on non-stenotic MCA and is promising for identification of BAD in SSIs.
Acknowledgements
This work was supported by the National Key Research and Development Program of China (No.2018YFC1312000), Tianjin Natural Science Foundation (No.20JCYBJC00960), Key Projects the National Science & Technology Pillar Program during the Twelfth Five-year Plan Period (No. 2011BAI08B09).References
[1] Sun et al. "High resolution magnetic resonance imaging in pathogenesis diagnosis of single lenticulostriate infarction with non-stenotic middle cerebral artery, a retrospective study." BMC neurology. 2018;18(1):51.
[2] Zhang, et al. "Visualization of the lenticulostriate arteries at 3T using black-blood T1-weighted intracranial vessel wall imaging: comparison with 7T TOF-MRA." European Radiology. 2019;29: 1452-1459.
[3] Kim, et al. “Secondary prevention by stroke subtype: a nationwide follow-up study in 46 108 patients after acute ischaemic stroke”. European Heart Journal.2013;34(35):2760–2767.
Figures