4144
Usefulness of low intensity rim sign on DWI for differentiating brain abscess, acute ischemic stroke, and hemorrhagic stroke.
Takashi Abe1,2, Maki Otomo2, Rintaro Ito1, Rei Nakamichi1, Yumi Abe1, Toshiki Nakane1, Hisashi Kawai1, Toshiaki Taoka1, Shinji Naganawa1, and Masafumi Harada2
1Nagoya University, Nagoya, Japan, 2Tokushima University, Tokushima, Japan
1Nagoya University, Nagoya, Japan, 2Tokushima University, Tokushima, Japan
Synopsis
Although it is often difficult to differentiate brain abscess, acute ischemic stroke, and hemorrhagic stroke on diffusion weighted image (DWI), the diagnosis can be made more accurately by focusing on the low signal intensity, especially the low intensity rim surrounding the lesion. In this study, image interpretation of six diagnostic radiologists (12.8 years of experience on average) showed an accuracy of 70% before explanation of the low intensity rim finding, but the accuracy increased to 86% after explanation (p = 0.025), confirming the importance of focusing on low intensity rim on DWI.
INTRODUCTION
The usefulness of diffusion-weighted imaging (DWI) for the diagnosis of acute ischemic stroke is widely known, and early diagnosis and early initiation of therapy lead to improved prognosis. It is important to diagnose correctly by DWI because that is the image firstly taken in the stroke MRI. However, both infarction and hemorrhage show hyperintensity on DWI, and their image findings are similar to those of brain abscess. Therefore, it is necessary to check other image sequence like T2*WI and MR angiography. However, because the low-intensity findings on DWI differ from each other in these diseases, attention to these findings may lead to a more accurate diagnosis using DWI alone. At this time, we tried to prove the usefulness of the low signal intensity on DWI for differentiating these diseases in this image interpretation study.METHOD
This retrospective study included 15 consecutive cases of untreated brain abscess diagnosed pathologically or clinically between 2012 and 2019. One patient was excluded because of a history of head surgery near the abscess. 20 consecutive cases of acute ischemic stroke and 26 consecutive cases of acute hemorrhagic stroke were collected. One representative DWI was selected from each case and 60 DW images were randomly classified into 2 groups. Six radiologists (7 to 20 years of experience) reviewed one group without any guidance and examined the accuracy of classification of brain abscess, cerebral infarction, and hemorrhage. The interpretation of another group was carried out after the following explanation; In brain abscesses, a thin, smooth, low-signal intensity rim surrounds the strong high-signal intensity. Cerebral hemorrhage is an irregular, heterogeneous mixture of high and low intensity on DWI, and the rim is nonuniform in thickness. The strong high signal can be also often recognized around the low intensity rim. In cerebral infarction, low signal rim is not observed, but in the basal ganglia, iron deposition may be seen as rim. The diagnostic accuracy before and after explanation was statistically analyzed and p-value less than 0.05 was considered significant.RESULT
Each diagnostic radiologist spent 14.8 minuites for the first reading (average, range: 10.5 -19.5 min.). The accuracy was 70.3% (average, range: 50 -80%). The reading time after the explanation about the low intensity rim sign was 7.3 min. (5.0 -8.5 min). The accuracy was increased to 85.8 % (70 -96.7 %, p = 0.025, paired t-test). The accuracy was correlated with years of experience of each radiologist (Pearson's correlation coefficient of 0.841, p = 0.036).DISCUSSION
Brain abscess, cerebral infarction, and cerebral hemorrhage show focal hyperintense lesion on DWI and their imaging findings are similar, but more accurate diagnosis was possible by focusing on low intensity rim surrounding the lesion. The mechanism of formation of low signal rim in brain abscess is considered to be the T2 shortening effect of free radical secreted from aggregated macrophages. On the other hand, the low signal intensity in the cerebral hemorrhage is mainly caused by the T2 shortening effect and the heterogeneity of the local magnetic field from the extracellular hemoglobin and deoxyhemoglobin. Because the low intensity is thought to originate from the displaced erythrocyte, the low signal rim at the periphery may also become serpentine and nonuniform in thickness, reflecting the heterogeneous formation of the hematoma. Although the high-intensity of DWI has attracted attention, the low-intensity is also considered to be useful for diagnosis.CONCLUSION
In the diagnosis of stroke MRI, not only the high signal intensity but also the low signal area on DWI can be used for more accurate diagnosis.Acknowledgements
No acknowledgement found.References
- Hiwatashi A, Kinoshita T, Moritani T, et al. AJR 2003; 181(6):1705-9
- Gomori JM, Grossman RI, Yu-Ip C, et al. JCAT. 1987;11(4):684-90.
Figures
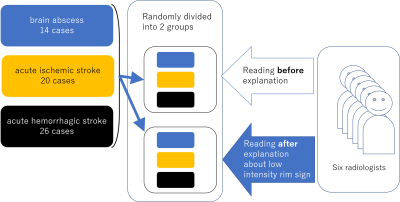
This retrospective study included
14 cases of untreated brain abscess, 20 cases of acute ischemic stroke and 26
cases of acute hemorrhagic stroke. One representative DWI was selected and
randomly divided into two groups. Six radiologists (7 to 20 years of
experience) reviewed one group consists of 30 DW image before any guidance. The
interpretation of another group was carried out after the explanation about the
characteristics of low intensity on DWI.
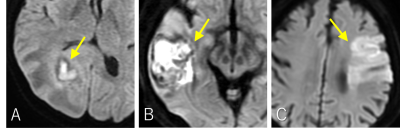
In brain abscesses, a thin, smooth, low-signal intensity rim surrounds the high-signal intensity (A). Cerebral hemorrhage is an irregular, heterogeneous mixture of high and low intensity on DWI, and the rim is nonuniform in thickness (B). The strong high signal can be also often recognized around the low intensity rim. In cerebral infarction, low signal rim is not observed (C), but in the basal ganglia, iron deposition may be seen as rim.
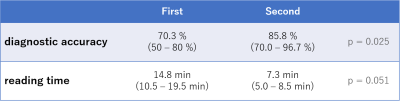
Data are presented as the; mean (range). Each diagnostic radiologist spent 14.8 min. for the first reading and the accuracy was 70.3%. The reading time after the explanation about the low intensity rim sign was 7.3 min. The accuracy was increased to 85.8 % (p = 0.025).