4138
FLAIR Vascular Hyperintensity May Predict Ischemic Event in Patients with Internal Carotid Artery or Middle Cerebral Artery Occlusion1Radiology, Chinese PLA General Hospital, The First Medical Center, Beijing, China
Synopsis
Intracranial artery steno-occlusive disease causes high morbidity of ischemic stroke occurrence and reoccurrence. The present study tested the presence of Fluid-Attenuated Inversion Recovery vascular hyperintensity (FVH) to discriminate symptomatic patients from asymptomatic patients in intracranial internal carotid artery or middle cerebral artery occlusion and found that the presence of FVH was independently associated with a recent ischemic event in these patients and negatively correlated with collateral circulation. The findings suggest that FVH may serve as a feasible imaging marker to identify high-risk cases in their follow-up and clinical management.
INTRODUCTION
Fluid-Attenuated Inversion Recovery Imaging (FLAIR) vascular hyperintensity (FVH) has been demonstrated correlation with hemodynamic impairments in intracranial artery steno-occlusive disease.1,2 The present study was to test whether the presence of FVH could be used to discriminate symptomatic patients from asymptomatic patients in intracranial internal carotid artery or middle cerebral artery occlusion.METHODS
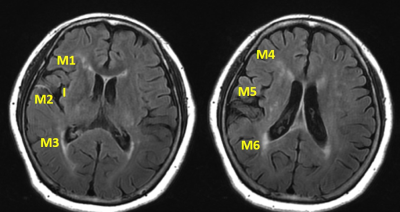
Patients with symptomatic and asymptomatic internal carotid artery or middle cerebral artery occlusion were prospectively enrolled. Patients were considered symptomatic if there was an ischemic stroke or transient ischemic attack present in the related territory within 90 days. Asymptomatic patients were included if there was no history of cerebrovascular events in the target downstream territory. Head routine MRI and arterial spin labeling (ASL) were performed on a 3.0T scanner. FVH-ASPECTS, a semi-quantitative scoring system for the evaluation of FVH robustness in accordance with insular and M1-M6 regions in Alberta Stroke Program Early Computed Tomography Score (ASPECTS) (illustrative case in Figure 1), was applied and assessed for each participant. FVH-ASPECTS 0 indicated the absence of FVH while FVH-ASPECTS 7 suggested prominent FVH. Then patients were categorized into FVH positive group (FVH-ASPECTS = 1-7) and FVH negative group (FVH-ASPECTS = 0).ASL collateral circulation grades, from 0 to 2 to indicate none collateral to favorable collaterals, were assessed based on the presence of arterial transit artifact (ATA) and hypoperfusion. Clinical and imaging characteristics were compared between patients with FVH and without. Multivariable logistic regression was conducted to select independent features associated with a recent ischemic event in these patients. Receiver-operating characteristic (ROC) analyses were performed to evaluate and compare the value of FVH positive and ASL collateral circulation in predicting the recent ischemic event. Linear regression was also performed to explore the relation between FVH-ASPECTS and ASL collateral circulation grade.RESULTS
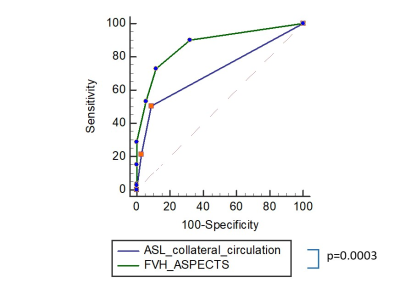
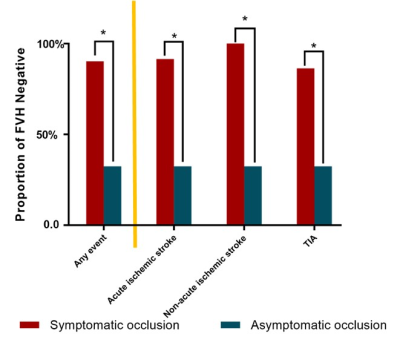
137 patients with 34 asymptomatic and 103 symptomatic ICA or MCA occlusion were recruited. There were 71 MCA occlusion and 66 ICA occlusion. The mean time from symptom onset to MRI was 11.69 ± 16.81 days. 33 cases showed FVH negative while 104 cases showed FVH positive. The proportion of symptomatic and asymptomatic occlusion, ASL collateral circulation grade, the proportion of females, and the frequency of smoking were significantly different between patients with and without FVH (p<0.05). Details are listed in Figure 2. The presence of FVH (odds ratio 13.409, 95% confidence interval 4.793 to 37.515, p<0.0001) and ASL collateral circulation grade (odds ratio 0.276, 95% confidence interval 0.102 to 0.750, p = 0.012) was significantly associated with recent ischemic event after adjusted by sex and smoking in multivariate logistic regression. The area under the curve (AUC) of FVH positive to predict recent ischemic events was 0.875 (95% confidence interval 0.806 to 0.926), which was significantly outperformed ASL collateral circulation grade (AUC 0.714, 95% confidence interval 0.629 to 0.789). Figure 3 presents the ROC comparison. The proportion of FVH positive was significantly lower in asymptomatic patients than in symptomatic patients, as well as than in subgroups of TIA, acute ischemic stroke, and non-acute ischemic stroke (Figure 4). Linear regression analysis revealed that lower FVH-ASPECTS correlated with more favorable ASL collateral circulation (r=0.46, p<0.001).CONCLUSION
The presence of FVH is associated with its likelihood to have caused a recent ischemic event in patients with internal carotid artery or middle cerebral artery occlusion, which suggests FVH may serve as a feasible imaging marker to identify high-risk cases in their follow-up and thereby to improve the management of primary and secondary prevention.Acknowledgements
NoneReferences
1.Mahdjoub E, Turc G, Legrand L, et al. Do Fluid-Attenuated Inversion Recovery Vascular Hyperintensities Represent Good Collaterals before Reperfusion Therapy? Am J Neuroradiol. 2018;39(1):77–83.
2.Nave AH, Kufner A, Bücke P, et al. Hyperintense Vessels, Collateralization, and Functional Outcome in Patients With Stroke Receiving Endovascular Treatment. Stroke. 2018;49(3):675–681.
Figures