4133
3D high resolution CUBE imaging in evaluating the imaging features of intracranial vasculopathy long after cranial irradiation1The First Affiliated Hospital of Shandong First Medical University, Jinan, China, 2GE Healthcare, MR Research China, Beijing, P.R. China, Beijing, China
Synopsis
The purpose of this study was to evaluate the imaging characteristics of intracranial large and small vessel diseases long after cranial irradiation. All patients with small vessel diseases underwent intracranial vessel wall imaging by 3D high resolution CUBE T1-weighted imaging (HR-MRI) to detect large vessel diseases. All recruited patients were found with intracranial small and large vessel diseases. Therefore, intracranial vasculopathy is not a rare complication after cranial irradiation, even in young patients. Patients after cranial irradiation should be followed up with MR imaging including HR-MRI.
INTRODUCTION
Radiation-induced neuropathy is commonly observed among oncological patients. Cranial irradiation can affect the nervous tissue directly or indirectly by inducing intracranial vasculopathy comprising of cerebral small and large vessel diseases. Recently, small vessel diseases after cranial irradiation has attracted attention as an important radiation-induced cerebrovascular disease1. Many cases of intracranial large artery stenosis as late complications of radiotherapy were described in previous studies2. However, few studies have focused on the evaluation of the characteristics of both small and large vessel diseases long after cranial irradiation. Moreover, vessel wall imaging features of radiation-induced intracranial large vessel diseases were also seldom studied. Therefore, this study aimed to assess radiation-induced cerebral small vessel damages, including microbleeds (MBs), lacunar infarctions (LI), or white matter hyperintensities (WMH) by using conventional brain MRI and large vessel diseases regarding vessel wall thickening and enhancement patterns by using 3D high resolution CUBE T1-weighted imaging (HR-MRI).MATERIALS AND METHODS
SubjectsWe included 7 patients (mean age: 57.7 years old, ranged from 44 to 76 years old), who were found to have intracranial artery stenosis (>50%) at least 5 years after radiation therapy for intracranial tumors. Each patient underwent conventional brain MRI and HR-MRI.
MRI experiments
All experiments were performed on a 3T clinical scanner (Discovery 750w, GE Healthcare, Milwaukee, WI, USA) equipped with a 32-channel coil. Conventional brain MRI comprised of a complete set of T1W, T2W, FLAIR imaging, susceptibility-weighted imaging (SWI) and magnetic-resonance-angiography (MRA).
Both plain and enhanced fast-spin-echo based 3D T1-weighted CUBE technique was employed for each patient. The corresponding scan parameters include: TR=600ms; TE=14.4ms; slice thickness=1mm; slice gap=0.5mm; FOV=200mm×200mm for whole brain coverage; matrix size=288×288 and echo length train=24. Gd-DTPA (0.1 mmol/kg) was administrated intravenously, and 3D CUBE T1-weighted HR-MRI was repeated 2 minutes after contrast material administration. Total scanning time was 8 minutes 32s.
Image analysis
All brain images were reviewed by two experienced radiologists. MBs were identified as small circular or ellipsoidal hypointense signals that were less than 10mm in maximum diameter on SWI. LI were defined as parenchymal defects ≤15mm in diameter in the regions of perforating arteries; they were hyperintense on FLAIR imaging or T2W or hypointense on T1W. WMH were identified as periventricular, peri-lesion or deep white matter hyperintensities on FLAIR imaging or T2W.
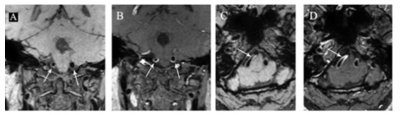
Eccentric wall thickening on HR-MRI was defined as the eccentricity index was ≥0.5, while for concentric thickening, this index was<0.5. The eccentricity index calculated by the formula: {(maximal thickness-minimal thickness)/maximal thickness}. The pattern of enhancement was rated as focal or circle enhancement. The degree of enhancement was categorized as none (equivalent to normal wall), moderate (less than the infundibulum enhancement), prominent (greater than the infundibulum enhancement). Train track sign was defined as complete vessel wall enhancement like parallel train track. Both radiologists were asked to assess the whole intracranial artery segments.
Data analysis
For categorical variables, the Cohen’s kappa coefficient was used to assess the inter-observer agreement between both radiologists. Statistical analyses were performed with SPSS 22.0 version software.
RESULTS
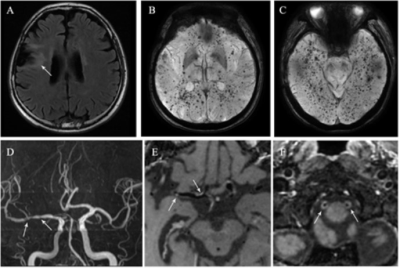
In this study, the Cohen’s kappa coefficient was separately applied to estimate the inter-agreement of conventional brain MRI and HRMRI between two radiologists. High Kappa values were obtained for T1W(0.935)、T2W(0.941)、FLAIR imaging(0.922)、SWI(0.912) and HR-MRI(0.901) .MBs were detected in 6 of 7 patients (85.7%). Among them, MBs in one patient located all over the brain. WMH were detected in 6 patients and the number of LI were 6 in two patients. These imaging features strongly suggest small vessel damages.
Seventeen lesions of intracranial artery segments which comprised of five luminal occlusive lesions and twelve luminal stenotic lesions were observed on HR-MRI. Among twelve intracranial stenotic lesions, seven lesions had an appearance of concentric wall thickening, three were eccentric wall thickening, one had an appearance consistent with intraluminal thrombus, and one was normal on pre-contrast T1W HR-MRI. Three of the seven lesions with concentric wall thickening didn’t show arterial wall enhancement on post-contrast HR-MRI, whereas the remaining four lesions had prominent circle enhancement, corresponding with train track sign, indicating arteritis. All three lesions with eccentric wall thickening had an appearance, being consistent with focal enhancement of the arterial wall on post-contrast HR-MRI, suggesting atherosclerosis.
DISCUSSION
In this study, all 7 patients were found with intracranial small and large vessel diseases. Two mechanisms of irradiation-induced vascular damages have been proposed: One is the acceleration of atherosclerosis, which mainly results in intimal thickness, and the other is endothelial cell injury of large and small vessels3. Blood-brain-barrier disruption in capillaries due to the vulnerability of endothelial cells to radiation injury may be responsible for multiple microbleeds. In addition, the damaged endothelial cells of large arteries cannot guard against plasma lipoproteins, allowing lipid infiltration and subsequent intimal plaque formations, gradually presenting as vulnerable plaques4.CONCLUSION
In conclusion, both cerebral small and large vessel diseases existed in patients long after cranial irradiation. Intracranial vasculopathy is not a rare complication after cranial irradiation, even in young patients. Patients after cranial irradiation should be followed up with MR imaging including HR-MRI.Acknowledgements
We thank Weiqiang Dou from GE Healthcare for this valuable support on the 3D-CUBE T1 vessel wall sequence.References
1. Miura M, Nakajima M, Fujimoto A, Ueda A, Watanabe M, Ando Y. Rinsho Shinkeigaku. 2015;55(10):743-747.
2. Nordstrom M, Felton E, Sear K, et al. Large Vessel Arteriopathy After Cranial Radiation Therapy in Pediatric Brain Tumor Survivors. J Child Neurol. 2018;33(5):359-366.
3. Plummer C, Henderson RD, O'Sullivan JD, Read SJ. Ischemic stroke and transient ischemic attack after head and neck radiotherapy: a review. Stroke. 2011;42(9):2410-2418.
4. Grenier Y, Tomita T, Marymont MH, Byrd S, Burrowes DM. Late postirradiation occlusive vasculopathy in childhood medulloblastoma. Report of two cases. J Neurosurg. 1998;89(3):460-464.
Figures