4083
Clinical value of MAVRIC-SL MRI for the assessment of periprosthetic joint infection1Radiology, Toho University Sakura Medical Center, Sakura, Japan
Synopsis
MAVRIC-SL enabled to improve the image quality by decreasing susceptibility artifacts and the assessment of periprosthetic joint infection after joint arthroplasty. Joint effusion, soft-tissue fluid collection, and soft-tissue edema were suggestive of periprosthetic joint infection. Soft-tissue fluid collection and soft-tissue edema were indicative of therapeutic surgical intervention for periprosthetic joint infection. Using MAVRIC-SL, MRI can become a useful tool to suggest periprosthetic joint infection in arthroplasty patients and to determine the management of periprosthetic joint infection.
Introduction
Implantation of joint prostheses is becoming increasingly common in the world. Infection is the most devastating of prosthesis-related complications and the infection rates might have been higher than previously reported1,2. There has been a demand for imaging modalities that can provide an accurate postoperative assessment after implantation of joint prostheses. Recently, advanced metal artifact reduction (MAR) sequences including MAVRIC, SEMAC, and MAVRIC-SL have been proposed to improve image quality by reducing susceptibility artifacts in patients with metal implant3. To our knowledge, however, there are a few reports evaluating periprosthetic joint infection (PJI) using the advanced MAR sequences4,5. The purpose of this study was to assess the clinical value of MAVRIC-SL MRI for PJI.Methods
44 joints in 33 patients after joint replacement underwent MRI including 2D FSE and MAVRIC-SL were enrolled (28 females, five males; age range, 55-92years; 29 hip, 13 knee, two elbow). All MRI was performed with a 1.5-T system (Optima MR450W, GE Healthcare). 2D FSE was obtained with PD- or T2WI, followed by STIR or FS-T2WI, and T1WI. MAVRIC-SL was obtained with STIR, followed by PDWI. The image quality on 2D FSE and MAVRIC-SL was assessed by two radiologists. The abnormal findings including joint effusion, soft-tissue fluid collection, soft-tissue edema, abnormal signal intensity (SI) around implant, lymphadenopathy, and other abnormal findings were assessed. Regarding the soft-tissue fluid collection, communication with the joint and surrounding capsular-like structure were assessed. Clinical data and final diagnosis were recorded. Sensitivities, specificities, accuracies, positive predictive values (PPV), negative predictive values (NPV), and odds ratios (OR) to suggest PJI and to indicate therapeutic surgical intervention for PJI were calculated. P<0.05 indicated a statistically significant difference. The interobserver agreements were calculated.Results
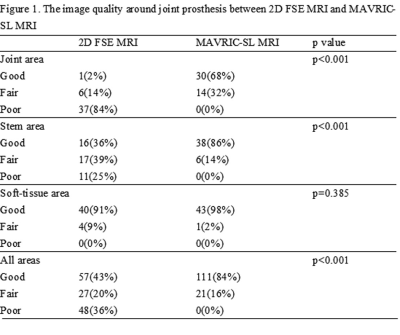
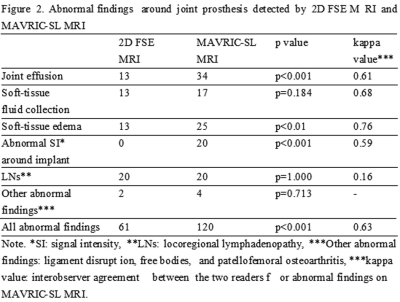
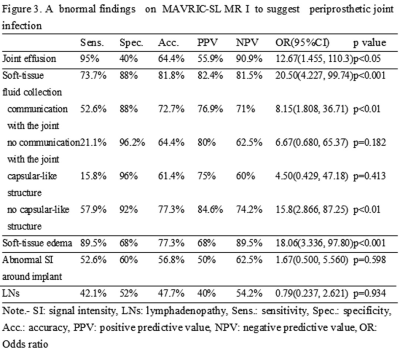
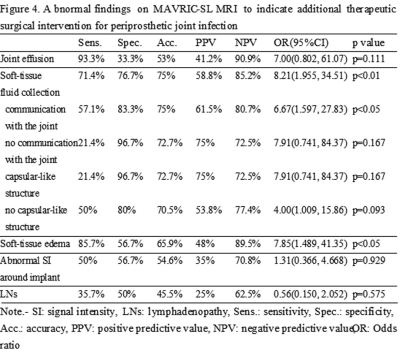
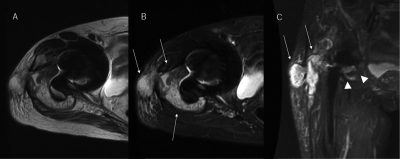
Out of the 44 joints, 19 (43%) were diagnosed as PJI and 14 underwent therapeutic surgical intervention for PJI. There were statistically significant differences in the image quality at the joint and stem areas, while there was no statistically significant difference at the soft-tissue area between 2D FSE and MAVRIC-SL (Fig.1). The abnormal findings around joint prosthesis were better detected by MAVRIC-SL than by 2D FSE (Fig.2). In the 19 joints with PJI, 19 had joint effusion, 17 had soft-tissue edema, 14 had soft-tissue fluid collection, 10 had abnormal SI around implant, and 8 had lymphadenopathy. Sensitivities, specificities, accuracies, PPVs, NPVs, and ORs of the abnormal findings to suggest PJI and to indicate therapeutic surgical intervention for PJI were expressed on Figs.3 and 4.Discussion
In our study, joint effusion was the most frequent on MAVRIC-SL, which had a 95% sensitivity, a 40% specificity, and a 90.9% NPV. Galley5 reported that joint effusion on SEMAC was not suggestive of PJI after hip arthroplasty. Nardo6 reported that one of the most frequent abnormalities on MAVRIC-SL after hip arthroplasty was joint effusion. Therefore, we consider that joint effusion is commonly seen in arthroplasty patients on MAVRIC-SL, but it has a high NPV for detection of PJI. Soft-tissue fluid collection and edema on MAVRIC-SL suggested PJI in our study. Soft-tissue fluid collection with communication with the joint or with no capsular-like structure suggested PJI. Galley5 reported that capsule and muscle edema after hip arthroplasty had a high accuracy for evaluation of PJI on SEMAC. Cyteval7 reported that abnormal findings in soft-tissue on CT were accurate for detection of PJI after hip arthroplasty, where fluid collection in muscles and perimuscular fat had a 100% PPV for PJI. Berquist8 reported that bursa-like cavities were frequently seen around the hip on arthrography for pain after hip arthroplasty and the infected ones were more irregular, with frequently a narrow, irregular neck. van Holsbeeck9 reported that joint effusion with extraarticular extension on sonograms suggested PJI. Their studies are supportive of our results. Abnormal SI around implant was not suggestive of PJI and the interobserver agreement was fair in our study. Choi10 reported that MAVRIC-SL enabled visualization of bone-metal interface in hip arthroplasty by reducing susceptibility artifact, but the interobserver agreement was fair. So, correlation with radiographs should be required for periprosthetic evaluation. We agree that it should be paid attention to interpret periprosthetic findings even on MAR MRI. Albano11 reported that lymph nodal indices on MRI represented biomarkers of infection after hip arthroplasty. Isern-Kebschull12 reported that enlarged iliac lymph nodes on CT after hip arthroplasty suggested PJI. In our study, however, lymphadenopathy on MAVRIC-SL was not suggestive of PJI and the interobserver agreement was poor. The abnormal findings to indicate therapeutic surgical intervention for PJI were soft-tissue fluid collection and edema in our study. Soft-tissue fluid collection with communication with the joint indicated therapeutic surgical intervention. There was a close relation between soft-tissue fluid collection and edema. So, we consider that the soft-tissue fluid collection is the most important to indicate therapeutic surgical intervention.Conclusion
MAVRIC-SL enabled to improve the image quality by decreasing susceptibility artifacts and the assessment of PJI after joint arthroplasty. Joint effusion, soft-tissue fluid collection, and soft-tissue edema were suggestive of PJI. Soft-tissue fluid collection and edema were indicative of therapeutic surgical intervention for PJI. Using MAVRIC-SL, MRI can become a useful tool to suggest PJI in arthroplasty patients and to determine the management of PJI.Acknowledgements
No acknowledgement found.References
1. Kurtz S, Ong K, Lau E, et al. Projections of primary and revision hip and knee arthroplasty in the united states from 2005 to 2030. J Bone Joint Surg Am, 2007;89:780-785
2. Kapadia B, Berg RA, Daley JA, et al. Periprosthetic joint infection. Lancet, 2016;387:386-394
3. Talbot BS, Weinberg EP. MR imaging with metal-suppression sequences for evaluation RadioGraphics, 2016;36:209-215
4. Li AE, Sneag DB, Greditzer HG, et al. Total knee arthroplasty: diagnostic accuracy of patterns of synovitis at MR imaging. Radiology, 2016;281:499-506
5. Galley J, Sutter R, Stern C, et al. Diagnosis of periprosthetic hip joint infection using MRI with metal artifact reduction at 1.5T. Radiology, 2020;296:98-108
6. Nardo L, Han M, Kretschmar M, et al. Metal artifact suppression at the hip: diagnostic performance at 3.0T versus 1.5Tesla. Skeletal Radiol, 2015;44:1609-1616
7. Cyteval C, Hamm V, Sarrabere MP, et al. Painful infection at the site of hip prosthesis: CT imaging. Radiology, 2002;224:477-487
8. Berquist TH, Bender CE, Maus TP, et al. Pseudobursae: a useful finding in patients with painful hip arthroplasty. AJR Am J Roentgenol, 1987;148:103-106
9. van Holsbeeck MT, Eyler WR, Sherman LS, et al. Detection of infection in loosened hip prostheses: efficacy of sonography. AJR Am J Roentgenol, 1994;163:381-384
10. Choi SJ, Koch KM, Hargreaves BA, et al. Metal artifact reduction with MAVRIC SL at 3-T MRI in patients with hip arthroplasty. AJR Am J Roentgenol, 2015;204:140-147
11. Albano D, Messina C, Zagra L, et al. Failed total hip arthroplasty: diagnostic performance of conventional MRI features and locoregional lymphadenopathy to identify infected implants. J Magn Reson Imaging, 2020
12. Isern-Kebschull J, Tomas X, Garcia-Diez AI, et al. Value of multidetector computed tomography for the differentiation of delayed aseptic and septic complications after total arthroplasty. Skeletal Radiol 2020, 49:893-902
Figures