4075
Detection of Sacroiliac Joint Lesions in Axial Spondyloarthritis:Utility of Synthetic MRI1Radiology, the Fifth Affiliated Hospital, Sun Yat-sen University, Zhuhai, China
Synopsis
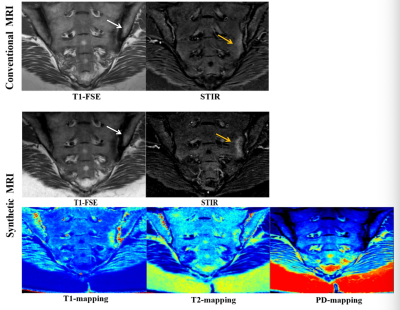
The current diagnosis of the sacroiliac joint lesions with axSpA is most concentrated on qualitative or semi-quantitative methods.There is an urgent need for a quantitative method that can objectively and accurately evaluate the severity of the disease.Synthetic MRI(MAGiC) can generate multiple contrast images and quantitative maps simultaneously based on the same scan.In this study the synthetic MRI can achieve similar qualitative diagnostic performance in detection of sacroiliac joint lesions compared with conventional MRI.And it could be used for distinguishing BME and fat metaplasia.
Acknowledgements
No acknowledgement found.References
1. Navallas, María, Ares, Jesús, Beltrán, Brigitte, et al. Sacroiliitis Associated with Axial Spondyloarthropathy: New Concepts and Latest Trends. Radiographics 2013;33(4):933-956.
2. Campochiaro C,Caruso P F.Ankylosing Spondylitis and Axial Spondyloarthritis. New Engl J Med 2016;375(13):1302.
3. Sieper J, Rudwaleit M, Baraliakos X, et al. The Assessment of SpondyloArthritis international Society (ASAS) handbook: a guide to assess spondyloarthritis. Ann Rheum Dis 2009;68(suppl 2):ii1–ii44.
4. Maksymowych WP, Wichuk S, Dougados M, et al. Mri evidence of structural changes in the sacroiliac joints of participants with non-radiographic axial spondyloarthritis even in the absence of MRI inflammation. Arthritis Res Ther 2017;19(1).
5. Maksymowych W P , Lambert R G , Stergaard M , et al. MRI lesions in the sacroiliac joints of participants with spondyloarthritis: an update of definitions and validation by the ASAS MRI working group. Ann Rheum Dis 2019;78 (11):1550-1558.
6. Braun J, Sieper J, Bollow M. Imaging of sacroiliitis. Clin Rheumatol 2000;19(1):51–57.
7. van den Berg R, Lenczner G, Thévenin F, et al. Classification of axial SpA based on positive imaging (radiographs and/or MRI of the sacroiliac joints) by local rheumatologists or radiologists versus central trained readers in the DESIR cohort. Ann Rheum Dis 2015;74:2016–21.
8. van den Berg R, de Hooge M, van Gaalen F, et al. Percentage of participants with spondyloarthritis in participants referred because of chronic back pain and performance of classification criteria: Experience from the spondyloarthritis caught early (SPACE) cohort. Rheumatology (Oxford) 2013;52:1492–9.
9. Poddubnyy D,et al.Brief Report: Course of Active Inflammatory and Fatty Lesions in participants With Early Axial Spondyloarthritis Treated With Infliximab Plus Naproxen as Compared to Naproxen Alone: Results From the Infliximab As First Line Therapy in participants with Early Active Axial Spondyloarthritis Trial.Arthritis Rheumatol 2016;68(8):1899–903.
10. Machado PM,et al.MRI vertebral corner inflammation followed by fat deposition is the strongest contributor to the development of new bone at the same vertebral corner: a multilevel longitudinal analysis in participants with ankylosing spondylitis. Ann Rheum Dis 2016;75(8):1486–93.
11. Gezmis E, Donmez FY, Agildere M. Diagnosis of early sacroiliitis in seronegative spondyloarthropathies by DWI and correlation of clinical and laboratory findings with ADC values. Eur J Radiol 2013;82(12):2316–2321.
12. Bradbury LA, Hollis KA, Gautier B, et al. Diffusion-weighted imaging is a sensitive and specific magnetic resonance sequence in the diagnosis of ankylosing spondylitis. J Rheumatol 2018;45(6):771–778.
13. Zhang P, Yu K, Guo R, et al. Ankylosing spondylitis: correlations between clinical and MRI indices of sacroiliitis activity. Clin Radiol 2015;70(1):62–66.
14. Lee KH, Chung HY, Xu X, Lau VWH, Lau CS. Apparent diffusion coefficient as an imaging biomarker for spinal disease activity in axial spondyloarthritis. Radiology 2019;291:121–128.
15. Guermazi, Ali, Roemer, Frank W. Which Is Better for Characterizing Disease Activity in Axial Spondyloarthritis: Diffusion MRI or T2-weighted/STIR MRI?. Radiology 2019;291:1, 129-130.
16. Kucybaa I , Ciuk S , Urbanik A , et al. The usefulness of diffusion-weighted imaging (DWI) and dynamic contrast-enhanced (DCE) sequences visual assessment in the early diagnosis of axial spondyloarthritis. Rheumatology International 2019;39(2):1559–1565.
17. Mi K K , Hong C S , Moonjung H , et al. Application of Synthetic MRI for Direct Measurement of Magnetic Resonance Relaxation Time and Tumor Volume at Multiple Time Points after Contrast Administration: Preliminary Results in participants with Brain Metastasis. Korean Journal of Radiology 2018;19(4):783-791.
18. W. Krauss, M. Gunnarsson, M. Nilsson, P. Thunberg. Conventional and synthetic MRI in multiple sclerosis: a comparative study. Eur. Radiol 2018;28:1692–1700.
19. Tanenbaum X L N , Tsiouris X A J , Johnson X A N , et al. Synthetic MRI for Clinical Neuroimaging: Results of the Magnetic Resonance Image Compilation (MAGiC) Prospective, Multicenter, Multireader Trial. Am. J. Neuroradiol 2017; 38 (6):1103-1110.
20. S.H. Lee, Y.H. Lee, H.T. Song, J.S. Suh, Quantitative T2mapping of knee cartilage:comparison between the synthetic MR imaging and the CPMG sequence, Magn.Reson. Med. Sci. 2018;17(4):344–349.
21. Kumar NM, Fritz B, Stern SE, Warntjes JBM, Lisa Chuah YM, Fritz J. Synthetic MRI of the Knee: Phantom Validation and Comparison with Conventional MRI. Radiology 2018;289(2):465–477.
22. S. Boudabbous, A. Neroladaki, I. Bagetakos, M. Hamard, B.M. Delattre, M.I. Vargas. Feasibility of synthetic MRI in knee imaging in routine practice. Acta Radiol. Open 2018;7(5):1–9.
23. M.I. Vargas, M. Drake-Pérez, B.M.A. Delattre, J. Boto, K.O. Lovblad, S. Boudabous, Feasibility of a synthetic MR imaging sequence for spine imaging, Am. J. Neuroradiol 2018;39 (9):1756-1763.
24. M. Drake-Pérez, B.M.A. Delattre, J. Boto, A. Fitsiori, K.O. Lovblad, S. Boudabbous, M.I. Vargas, Normal values of magnetic relaxation parameters of spine components with the synthetic MRI sequence. Am. J. Neuroradiol 2018; 39 (4): 788-795.
25. Roux M, Hilbert T, Hussami M, Becce F, Kober T, Omoumi P. MRI T2 Mapping of the Knee Providing Synthetic Morphologic Images: Comparison with Conventional Turbo Spin-Echo MRI. Radiology 2019;293:620–630.
26. Fritz J . T2 Mapping without Additional Scan Time Using Synthetic Knee MRI. Radiology 2019;293(3):192046.
27. Zhan Y, Jiang Y, Zhang K,et al. Feasibility study on application of MAGiC sequence in sacroiliac joint of young volunteers. Chin J Magn Reson Imaging 2020;11(7):568-72.
28. Maksymowych W P , Inman R D , Salonen D , et al. Spondyloarthritis research Consortium of Canada magnetic resonance imaging index for assessment of sacroiliac joint inflammation in ankylosing spondylitis.Arthritis Rheum 2005;53(4):502-509.
29. Warntjes JB, Dahlqvist O, Lundberg P. Novel method for rapid, simultaneous T1, T2*, and proton density quantification. Magn Reson Med 2007;57(3):528–537.
30. Warntjes JB, Leinhard OD, West J, Lundberg P. Rapid magnetic resonance quantification on the brain: optimization for clinical usage. Magn Reson Med 2008;60(2):320–329.
31. Zhu DC, Penn RD. Full brain T1 mapping through inversion-recovery fast spin echo imaging with time-efficient slice ordering. Magn Reson Med 2005;54:725–731.
32. Lee SM, Choi YH, Cheon JE, et al. Image quality at synthetic brain magnetic resonance imaging in children. Pediatr Radiol 2017;47:1638 –47.
33. Wang D , Yin H , Liu W , et al. Comparative analysis of the diagnostic values of T2 mapping and diffusion-weighted imaging for sacroiliitis in ankylosing spondylitis. Skeletal Radiology 2020; 2:1-10.
34. Jiang, Yuwei et al.Quantitative synthetic MRI for evaluation of the lumbar intervertebral disk degeneration in participants with chronic low back pain. Eur J Radiol 2020;124:108858.
35. Puhakka KB, Jurik AG, Egund N, et al. Imaging of sacroiliitis in early seronegative spondylarthropathy: assessment of abnormalities by MR in comparison with radiography and CT. Acta Radiol 2003;44(2): 218–229.
Figures