4018
Subject-specific positional probability volume mapping for internal target volume determination in Radiotherapy
Oi Lei Wong1, Jing Yuan1, Darren MC Poon2, Yi Hang Zhou1, Siu Ki Yu1, and Kin Yin Cheung1
1Medical Physics and Research, Hong Kong Sanatorium, Hong Kong, Hong Kong, 2Comprehensive Oncology Center, Hong Kong Sanatorium, Hong Kong, Hong Kong
1Medical Physics and Research, Hong Kong Sanatorium, Hong Kong, Hong Kong, 2Comprehensive Oncology Center, Hong Kong Sanatorium, Hong Kong, Hong Kong
Synopsis
A novel ITV determination technique based on the volume of positional probability distribution (PPV) generated by volumetric 4DMRI was proposed and verified on cancer patients. For large targets, both PPV and 4D-CT generated ITV were similar with relatively large DSC. For small targets, however, relatively small DSC was observed, where poor tumor visibility in 4D-CT may be the cause.
Purpose
Internal target volume (ITV) is defined to accommodate tumor motion in radiotherapy treatment planning (RTP), and is commonly determined based on 4D-CT images. But, the reliability of the 4D-CT determined ITV for cancer in the abdomen is much limited by the intrinsic low soft-tissue image contrast of CT and the short scan time (to minimize radiation burden), particularly for irregular respirations. By taking the advantages of the non-ionizing radiation nature of MRI as well as its superior soft-tissue image contrasts, 4D-MRI is anticipated to be a valuable tool for radiotherapy for ITV determination in treatment planning and inter-fractional ITV verification [1]. In this study, we propose a novel ITV determination technique based on the volume of the positional probability distribution (PPV) estimated using 4D-MRI.Image acquisition
4 abdominal cancer patients (3 males, 1 females, age = 68±16 years, 5 lesions) were recruited. 4D-CT images were acquired on a CT simulator with a camera system to monitor the abdominal AP shift as the external surrogate of respiratory motion (120kV, 50 mAs, 2mm slice thickness, scan time = 60~70s). The 4D-CT images were retrospectively sorted into 10 respiratory phases by the external respiratory surrogate system. The ITV was delineated by an oncologist to cover the gross target volume (GTV) on 4D-CT in all ten phases with respect to the mid-inhalation position. Free-breathing abdominal volumetric 4D-MRI were axially acquired on a 1.5T MR-simulator with same positioning and immobilization as 4D-CT (CAIPIRINHA-TWIST-VIBE, TE/TR=0.35/1.57ms, flip angle=5o, FOV=350-382mm, acquisition matrix size= 128x128; slices=52-64; slice-thickness=4.5-5mm; reconstruction voxel size=2.7x2.7x4.5 - 3.0x3.0x5.0mm3, phase FOV= 71.9%; partial Fourier factor=75% (phase encoding)/62% (slice encoding); slice over-sampling factor=20%; central and 33% peripheral K-space sampling percent by TWIST; frame-rate = 2.5-3.0 frame-per-second (fps); 144 time-frames, acceleration factor=4).PPV generation
GTV was masked on the first time frame of the 4D-MRI to generate the baseline anatomical segmentation (Seg1). Images at each frame j (j>1) were non-linearly registered to the first time frame to obtain the transformation matrix, which was applied to Seg1 for the generation of Segj. The positional probability (PP) of a voxel in the imaged volume was calculated by the number of time frames that a voxel had been occupied by the organ-of-interest divided by the total elapsed frames, as presented in Eq.1, where j denotes the time frame index, and M is the binary mask value of 1 (the voxel is occupied by Segj) or 0 (the voxel is not occupied by Segj). rPPj=(M1+...+Mj)x100%/j if Mj∈Segj, then Mj=1; if Mj∉Segj, then Mj=0 [Eq.1]Positional probability volume (PPV) was estimated based on the relative frequency of the voxels in the imaged volume being occupied by the organ-of-interest during the 4D-MRI scan, where rPPVj,threshold corresponds to the number of voxels with the PPj value larger than the pre-defined threshold.
Statistical analysis
Subject-specific PPV144,0% and PPV144,5% of the GTV were compared with the ITV using signed-rank test. The similarity between PPVs and ITV was also evaluated based on the dice similarity coefficient (DSC), the volumetric difference (DiffITV,i%) and Hausdorff distance (HD).Results and discussion
As illustrated in Table 1, the ITV determined by 4D-CT was generally larger than the PPV144,0% (mean DiffITV,0% = 23%) and rPPV144,5% (mean DiffITV,5% = 36%) derived from 4D-MRI, indicating the overestimation of respiratory motion by 4D-CT. Despite the small patient sample size, the volume difference between ITV and PPV144,0% and PPV144,5% were just marginally insignificant(p=0.0625). ITV and PPV were similar in larger tumors with relatively large DSC (>0.80), suggesting the efficacy of 4D-MRI for respiratory motion characterization. In contrast, small DSCs (<0.70) were found between the ITV and PPV in particular for small tumors, implying the possible inaccuracy of 4D-CT in respiratory motion estimation resulted from poor tumor visibility.Besides the small sample size, the study limited in the PPVs and ITV comparison based on the possibly different respiratory profiles, a common problem for all in vivo 4D-MRI studies. Further study is warranted to increase the sample size to strengthen statistical power, and to compare the PPV and the 4D-CT ITV with the same respiratory profile based on an MR-CT compatible motion phantom.
Conclusion
A novel volumetric 4D-MRI derived rPPV approach was proposed for ITV determination and preliminarily validated in a small cohort of real patients. This rPPV approach should be potentially useful in patient-specific ITV determination in abdominal precision radiotherapy.Acknowledgements
No acknowledgement found.References
[1] Paulson ES, Ahunbay E, Chen X, Mickevicius NJ, Chen GP, Schultz C, Erickson B, Straza M, Hall WA, Li XA. 4D-MRI driven MR-guided online adaptive radiotherapy for abdominal stereotactic body radiation therapy on a high field MR-Linac: Implementation and initial clinical experience. Clin Transl Radiat Oncol. 2020 May 15;23:72-79.Figures
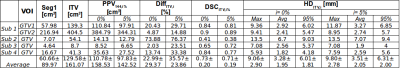
Table 1 The volume of ITV, PPV144,0% and PPV144,5% were tabulated. The dice similarity coefficient (DSCITV,i%), Hausdorff distance (HDITV,i%)and volumetric difference (DiffITV,i%) of the PPVs at i=0% and 5% referencing to the ITV from the treatment plan were also listed for each GTV.
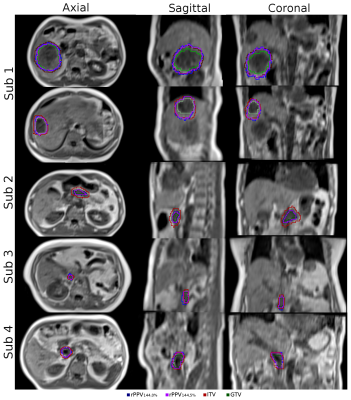
Figure 1 The contour of the rPPV144,0%, rPPV144,5%, ITV and GTV of all GTVs were denoted as blue, purple, red and green, respectively.