Jaime Mata1, Lauren Powlovich2, David Moore2, and Linda Martin1
1University of Virginia, Charlottesville, VA, United States, 2Focused Ultrasound Foundation, Charlottesville, VA, United States
Synopsis
Malignant lung cancer carries a poor prognosis with a 5-year
survival rate of about 18%. This new method proposes an innovative minimally
invasive procedure for the transcutaneous ablation of lung tumor masses with
complete removal or significant debulking of the masses. This new procedure
could increase lung cancer survival rates and at the same time decrease
morbidity and side effects associated with current treatment therapies. It will
also provide a viable treatment for a large group of patients that cannot
tolerate resection surgery, radiotherapy and chemotherapy, or who have had
prior radiation and cannot have additional radiation to that region.
Introduction
Malignant
lung cancer carries a poor prognosis (median survival of about 10 months) with
rare cases of complete cure and a 5-year survival rate of about 18 percent. Surgical
resection therapy was shown to have the greatest impact on survival and
consists of removing the entire lobe or segment of the affected region of the
lung, but unfortunately the majority of the lung cancer patients (about 60-70%)
do not qualify for or cannot tolerate surgery.
This method proposes an innovative minimally invasive
procedure for the transcutaneous ablation of lung tumor masses with complete
removal or significant debulking of the masses, without the use of traditional
open lung resection surgery. This technique does not require flooding of the
lung in order to get an acoustic window for the Focused Ultrasound (FUS), which
can pose serious immediate and long term risks for the patient (i.e. pneumonia,
sepsis, among other complications).Materials & Methods
Two Yucatan mini pigs (~30Kg) had both main bronchi
selectively intubated, and while the left lung was mechanically ventilated, the
right lung was purposely collapsed, followed by a controlled right hydrothorax
in the chest cavity with saline in order to create an acoustic window for the
FUS beam. At the end of the MR guided Focused Ultrasound (MRgFUS) ablation, the saline was drained in a method
identical to the drainage of a clinical pleural effusion. Animal #1 received
six transcutaneous MRgFUS ablations of the right lung, in six different
locations. Each location received a different amount of acoustic power in order
to determine the optimal power with minimal side effects (i.e. skin burns). Animal
#2 received two transcutaneous MRgFUS ablations on two large areas of the upper
lobe of the right lung. An intercostal approach was used in order to target the
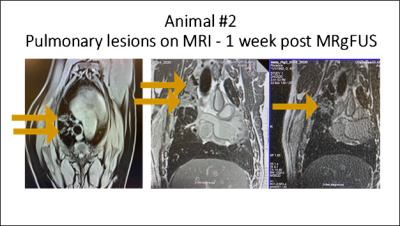
transcutaneous beam without distortion and attenuation caused by the ribs. One
week after the ablation, each animal received a MRI of the lung to assess the
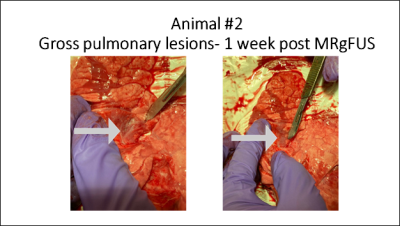
success of the ablation; animals were then euthanized and a histopathological examination
of the lungs was performed to correlate with the results of the MRI.Results
Ablations were done successfully on both animals. The
locations and sizes of the ablations as determined by post treatment MRI and
gross histology, correlated well with the initial target locations and the
power doses applied (Figs 1-2). The escalation test done on animal #1, was very
useful to determine the power and the duration of the treatments. This
information was used on animal #2 with immediate success (Figs 1-2) but further
refinement of the doses and treatment times is necessary to avoid skin lesions.
This should be accomplished in the near future on new animal studies.
Immediately after MRgFUS treatment, the saline in the chest
cavity was drained with only a small volume of ~10% (~60cc) remaining inside
the cavity. Both animals recovered very well from the MRgFUS treatment with no
significant side-effects besides a skin lesion on animal #2 at the place where
the transducer was located. Discussion
These
preliminary results are very encouraging. This new procedure could increase
lung cancer survival rates and at the same time decrease morbidity and side
effects associated with current treatment therapies like radiosurgery and
chemotherapy, since it will permit nonsurgical tumor ablation or tumor
debulking. It will also provide a viable treatment for a large group of
patients that cannot tolerate resection surgery, radiotherapy and chemotherapy,
or who have had prior radiation and cannot have additional radiation to that
region. For this large segment of the patient population, palliative care, not
full treatment, was traditionally the therapy of choice. The proposed procedure
may create new hope for these patients and improved palliation for others. Conclusion
Non-invasive ablation and debulking of lung tumors seems
possible with the novel method proposed using MRgFUS. We successfully ablated
lung tissue deep in the lung without incisions, reducing the risk for infection
and other complications.Acknowledgements
Supported in part by a grant from the Focused Ultrasound Foundation. References
No reference found.