3951
Motion Robust Parallel Transmission Excitation Pulse Design for Ultra-High Field MRI1Department of Physics and Astronomy, CUBRIC, Cardiff University, Cardiff, United Kingdom, 2Department of Psychology, CUBRIC, Cardiff University, Cardiff, United Kingdom
Synopsis
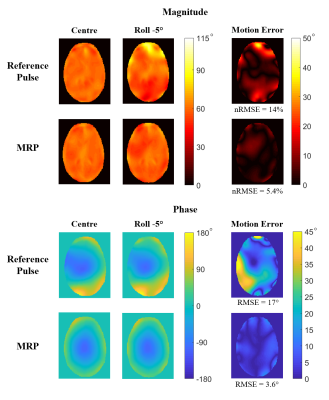
Within-scan patient motion reduces PTx pulse performance. A motion-robust PTx 5-spoke pulse (MRP) was designed using simulated B1 maps at multiple head positions, and was compared to a conventional 3-spoke reference pulse. For a 5° rotated head orientation, magnitude nRMSE was reduced from 14% to 5.4%, phase RMSE from 17° to 3.6°, maximum magnitude and phase errors from 64% to 20% and 68° to 15° respectively. Although a longer pulse duration, the MRP maintained similar magnitude nRMSE to the reference pulse at the centre, and superior performance in 97% of all four error metrics for 46 off-centre positions.
Introduction
Parallel transmission of RF waveforms (PTx) using multiple transmit channels can greatly improve excitation homogeneity at UHF.1 PTx pulses use patient specific B1-maps for improving the flip-angle homogeneity, however the inherent position-specific nature of these maps leads to a reduction in PTx performance in the presence of patient motion.2 To address this motion sensitivity, we developed motion robust pulses (MRPs) for rotation and translation of the head. The MRP design presented at ISMRM 20203 has been updated with spoke placement optimisation, improved phase consideration, and more comprehensive evaluation. Pulses are now evaluated over ± on-axis rotation, on-axis translation, and off-axis translation in the left-right anterior-posterior plane.Methods
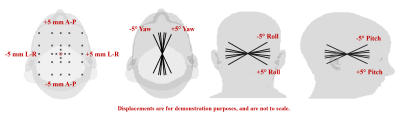
B1 maps of virtual body model Ella4 were simulated inside a generic 8-channel PTx coil using Sim4Life (Zurich MedTech, Zurich, CH) for 47 different positions of the body model (figure 1):- Central (no motion) case
- ±1°, ±2°, ±5° pitch/roll/yaw around-axis rotations (about the centre of the head)
- ±1mm, ±2mm, ±5mm left-right (L-R)/anterior-posterior (A-P) on-axis translations
- ±2mm, ±5mm L-R/A-P off-axis translations on the axial plane
For further detail please refer to figure(1) and Ref(2).
A 5-spoke MRP was designed combining the central and on-axis B1 map “extremes” (±5° pitch/roll/yaw, ±5mm L-R, ±5mm A-P), leading to 11 total design input positions. Pulse design was performed in patient coordinates by co-registering and concatenating all B1 maps while positional differences were incorporated by adapting gradient fields for each B1 map. The 5-spoke, small tip-angle, axial slice selective MRP was designed using an adapted spatial domain method.5 To maintain a consistent phase across positions, phase relaxation was removed. For each spoke, the ten best spokes were separately evaluated, yielding 10,000 pulses as the first spoke is always at kx = ky = 0 .
The target flip-angle was 60° with other pulse parameters the same as Ref(6).
The 5-spoke MRP was compared to a conventionally designed 3-spoke “reference” pulse, designed using the standard phase-relaxed spatial domain method (greedy spoke placement), and only the central B1 map.
Pulse performance was evaluated using four main error metrics, normalised root-mean-squared error (nRMSE) of the magnitude, maximum magnitude error, root-mean squared error (RMSE) of the phase, and maximum phase error. nRMSE in magnitude and RMSE in phase were calculated based on the error between each off-centre position and the central position. Magnitude and phase motion error profiles were produced by taking the absolute difference between off-centre profiles and the central profile.
Results
Figure (2) shows the -5° roll evaluation, the rotation receiving most benefit from the MRP. Compared to the reference pulse, the MRP reduced magnitude nRMSE from 14% to 5.4%, and phase RMSE from 17° to 3.6°. Maximum magnitude and phase errors were reduced from 64% to 20%, and 68° to 15° respectively, and were the largest reference pulse phase errors over all positions.The off-centre shift of -5 mm shift in the Left-Right axis (R-5), then shifted -5mm in the anterior-posterior axis (R-5 A-5) was the off-centre translation that benefitted most from the MRP, shown in figure (3). All error metrics were improved by the MRP, magnitude nRMSE was reduced from 10% to 4.8%, maximum magnitude error from 45% to 17%, phase RMSE from 9.5° to 3.9° and maximum phase error from 42° to 13°.
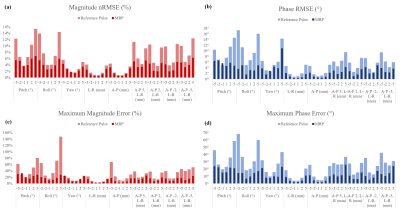
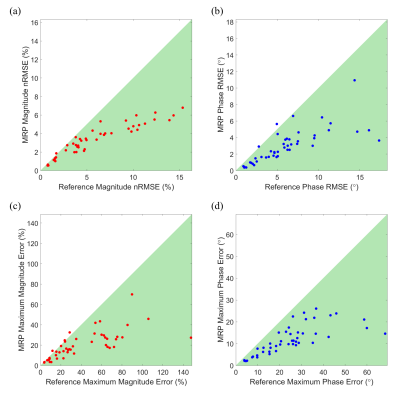
Figures (4,5) compare the four main error metrics of the reference pulse and the MRP over all evaluated positions. The MRP yielded superior performance in 97% of all error metrics (184 total) over all evaluated off-centre positions and very similar performance in remaining 3%. The maximum magnitude error reported overall was 148% for the reference pulse at 5° roll position, reduced to 27% by the MRP. The largest nRMSE recorded was 15.3% at the +5° pitch rotation for the reference pulse, reduced to 6.8% by the MRP.
The MRP yielded a similar magnitude nRMSE of 5.3% at the central position to the 5.0% of the reference pulse.
Discussion
The results presented demonstrate in-silico that motion-robust excitation pulses can be used as a method of maintaining highly homogeneous magnitude and phase profiles in the presence of patient-motion.Removing the phase-relaxed nature of the previous MRP design lead to much greater improvement in reducing motion-induced phase profile deterioration. This comes at the cost of slightly increased magnitude inhomogeneity, but is a necessary trade-off.
For equal number of spokes, the added complexity of improving the flip-angle and phase at multiple positions means the MRP cannot perform as well as the phase-relaxed conventional (reference) pulse when there is zero motion. Hence, we compared a 5-spokes MRP to 3-spokes conventional/reference pulse.
The MRP design could be improved further by considering a brute force algorithm for spoke placement. However, this is computationally intensive and currently can not be done in real-time. Alternatively, a library of k-space optimised MRPs can be designed offline for representative models. Then, the models that match the patient can be selected and applied, similar to Ref(7). This would also circumvent the requirement of multiple input B1 maps for the current MRP design.
Acknowledgements
No acknowledgement found.References
1. Zhu, Y. Parallel Excitation with an Array of Transmit Coils. Magn. Reson. Med. 51, 775–784 (2004).
2. Kopanoglu, E., Deniz, C. M., Erturk, M. A. & Wise, R. G. Specific absorption rate implications of within-scan patient head motion for ultra-high field MRI. Magn. Reson. Med. 84, 2724–2738 (2020).
3. Watkins, L., Plumley, A., Murphy, K. & Kopanoglu, E. Motion robust parallel transmission excitation pulse design for ultra-high field MRI. in ISMRM 2020 (2020).
4. Christ, A. et al. The Virtual Family - Development of surface-based anatomical models of two adults and two children for dosimetric simulations. Phys. Med. Biol. 55, (2010).
5. Grissom, W. et al. Spatial Domain Method for the Design of RF Pulses in Multicoil Parallel Excitation. 629, 620–629 (2006).
6. Grissom, W. A. et al. Advancing RF pulse design using an open-competition format: Report from the 2015 ISMRM challenge. Magn. Reson. Med. 78, 1352–1361 (2017).
7. Tomi-Tricot, R. et al. SmartPulse, a machine learning approach for calibration-free dynamic RF shimming: Preliminary study in a clinical environment. Magn. Reson. Med. 82, 2016–2031 (2019).
Figures