3944
Real-time tyGA Imaging for diagnosis and treatment evaluation of articular disc displacements in the TMJ1Department of Internal Medicine II, Ulm University Medical Center, Ulm, Germany, 2Department of Orthodontics, Ulm University Medical Center, Ulm, Germany
Synopsis
Magnetic resonance imaging (MRI) scans are the gold standard for confirming clinical diagnosis of temporomandibular disorders involving the condyle–articular disc complex, such as articular disc displacements (ADDs). Dynamic MRI has previously been applied for the visualization of motions of the temporomandibular joint. A combination of tiny golden angle (tyGA) profile ordering and a sliding window reconstruction allows retrospective reconstruction of images with nearly arbitrary temporal resolutions. In this contribution a real-time tyGA sequence with a frame rate of up to 125 ms was successfully applied for the diagnosis of ADD as well as occlusal splint therapy planning and evaluation.
Introduction
Magnetic resonance imaging (MRI) is a conventional approach for the diagnoses of disorders of the temporomandibular joint (TMJ), in particular for diagnosing articular disc displacements (ADDs)1. While static MRI images of the mouth in opened and closed positions provide only snapshots of the relative movements between the condyles and articular discs, dynamic imaging with high temporal resolutions can provide a detailed visualization of the course of the motion of the joint2.In this work we demonstrate the clinical feasibility of applying a real-time MRI sequence with tiny golden angle (tyGA) profile ordering scheme3, that allows to adapt the reconstructed temporal resolution to the respective requirements. Its application to the diagnosis of ADDs and the subsequent investigation of condyle and articular disc position during and after occlusal splint therapy was tested.
Methods
All data were acquired with a 3T whole-body clinical imaging system (Ingenia CX, Philips Healthcare, The Netherlands) using a 16-channel head-neck coil (Philips Healthcare). In vivo scans of the left and right TMJ were acquired from a patient, who reported locking of the mandible in a posterior position and periodic bruxism, headaches, and neck pain. The patient underwent functional and manual diagnostic testing for TMDs in accordance with the guidelines of the German Association for Functional Diagnostics and Therapy (DGFDT) before the MRI scans.Dynamic MRI scans of the left and right TMJs were acquired with a two-dimensional balanced steady‐state free precession (bSSFP) radial sequence using tyGA profile ordering with an angular increment of . Combined with a sliding window approach, the tyGA profile ordering scheme with its uniform coverage of k‐space allows retrospective reconstruction of images with nearly arbitrary temporal resolutions. The dynamic scans were reconstructed with a temporal resolution of 500ms and a temporal overlap of 250ms between subsequent frames. To improve visualization of the repositioning of the discs, an additional reconstruction with a temporal resolution of 245ms and an overlap of 125ms performed. The other scan parameters were as: field of view (FOV) = 180x180×5mm, resolution = 0.75×0.75x5mm, TR/TE = 4/2ms, flip angle = 45°, scan duration = 25s and an overall examination time of 15 minutes. Undersampled data were reconstructed using an iterative SPARSE-SENSE algorithm as part of an in-house software package implemented with MATLAB (MathWorks; Natick, MA, USA).
Imaged slices were obtained in an oblique sagittal orientation centered through the condylar head and the patient was instructed to uniformly open and close their mouth over a duration of 10s each with the following mandibular opening movements:
- The first jaw-opening movement started in maximum intercuspation, with a reduced mouth-opening due to TMJ locking.
- The second movement started from a protrusive mandibular position, enabling full opening of the mandible with repositioning of the condyles and articular discs.
- Finally, the mandibular occlusal splint was incorporated, and mandibular opening started with contact between the splint and maxillary teeth.
Results
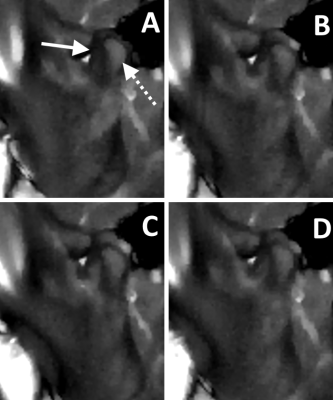
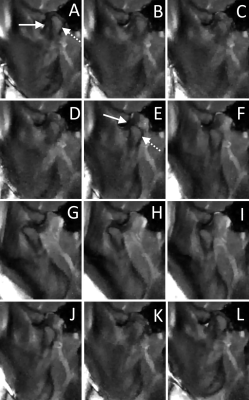
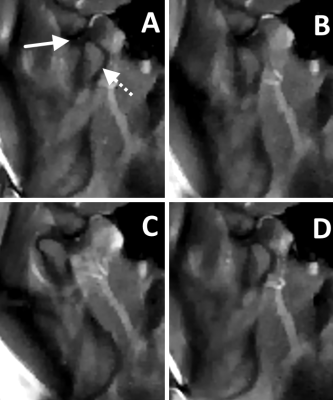
Figure 1 illustrates the dynamic MRI scan of jaw-opening from the position of habitual occlusion of the left TMJ and shows that the condyle (dotted arrow) remained locked behind the disc (solid arrow) after the rotational movement. The repositioning of the condyle on the disc is depicted in Figure 2, which occurred during the initial protrusive mandibular movement.Figure 3 shows, that after insertion of the occlusal splint both condyles were already in a therapeutic, more anterior and caudal initial position on the discs. The subsequent opening movement starting from this position showed no sign of any further disc displacement or repositioning.
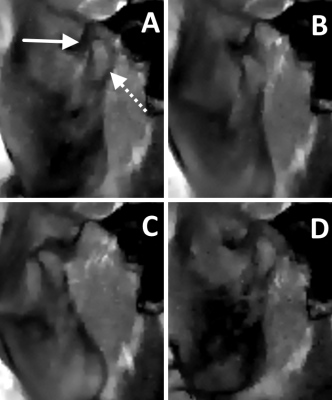
The follow-up MRI scan without splint, depicted in Figure 4, showed a stable repositioning of both condyles without any disc displacement occurring during the jaw movement. Moreover, no clicking was noticeable during the opening movement, and the patient’s clinical symptoms appeared considerably reduced.
Discussion and conclusion
Dynamic radial tyGA MRI scans with a frame rate of 250ms could confirm the initial diagnosis of an ADD in the right and left TMJs. While static MRI of the patient in habitual occlusion and with widely opened jaws are usually sufficient for the diagnosis of ADD without reduction, in the case of ADD with reduction (as exhibited by our patient), purely static MRI would not have provided sufficient information for treatment planning, as the exact timing of the reduction in the joint would have remained unknown. Using the tyGA profile ordering allowed to retrospectively reconstruct images with a higher frame rate of 125ms for an even more detailed visualization of the disc repositioning process. This also allowed to observe whether the condyles exhibit repositioning after insertion of a splint and the possible need for it to be adjusted.In conclusion, the feasibility of using a real-time MR sequence for diagnosing and therapeutic decision-making in case of ADD with reduction was demonstrated, showing the advantage of tyGA profile ordering to individually adapt the temporal resolution of the reconstructed images to the respective situation.
Acknowledgements
The authors thank the Ulm University Center for Translational Imaging MoMAN for its support Technical support from Philips Healthcare is gratefully acknowledged.References
[1] Schiffman E, Ohrbach R, Truelove E, Look J, Anderson G, Goulet JP, et al. Diagnostic criteria for temporomandibular disorders (DC/TMD) for clinical and research applications: recommendations of the international RDC/TMD consortium network and orofacial pain special interest group. J Oral Facial Pain Headache 2014; 28: 6–27.
[2] Abolmaali ND, Schmitt J, Schwarz W, et al. Visualization of the articular disk of the temporomandibular joint in near-real-time MRI: feasibility study. Eur Radiol. 2004;14:1889–1894
[3] Wundrak S, Paul J, Ulrici J, Hell E, Rasche V. A small surrogate for the golden angle in time-resolved radial MRI based on generalized fibonacci sequences. IEEE Trans Med Imaging 2014;34.
Figures