3942
Semiautomated quantitative analysis of swallow function using dynamic MRI with image registration and intensity analysis1Centre for Medical Imaging, University College London, London, United Kingdom, 2Department of Imaging, University College London Hospital, London, United Kingdom, 3Medical Physics, University College London Hospital, London, United Kingdom, 4Head and Neck Academic Centre, University College London, London, United Kingdom
Synopsis
Swallowing dysfunction (dysphagia) is a common problem and a major cause of morbidity in patients who have undergone radiotherapy for head and neck cancer. However, the pathophysiological basis of dysphagia in these patients is poorly understood and may differ between patients, creating a barrier to developing effective treatment strategies. Improved (and ideally quantitative) methods for characterising swallow function are therefore needed. We describe a method for imaging and analysis of pharyngeal and laryngeal motion during the swallow, based on joint image registration and modelling of intensity changes over a dynamic image series.
Introduction
Swallowing dysfunction (dysphagia) is a common problem and is particularly problematic in patients who have undergone radiotherapy for head and neck cancer. In these patients, dysphagia is thought to arise due to fibrosis of the laryngopharyngeal musculature and loss of sensation at the tongue base, leading to defective swallow triggering [1,2]. However, there is a lack of understanding of the exact contributing factors to swallowing dysfunction in individual patients, limiting efforts to develop effective treatments. Existing swallow assessment methods such as fibreoptic endoscopic evaluation of swallowing (FEES) and video fluoroscopic swallowing exam (VFS) provide useful information but are limited to qualitative or semiquantitative evaluation and provide only indirect information on swallowing mechanics, since the structures (muscles, ligaments and bone) involved in execution of swallowing are not directly imaged. We describe a method for imaging and semi-automated quantitative analysis of swallow function based on joint registration and modelling of intensity changes over a series of images acquired at high temporal resolution during swallowing.Methods
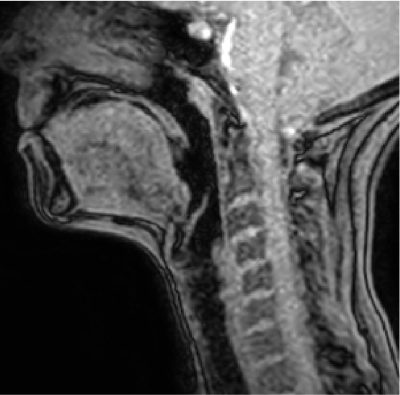
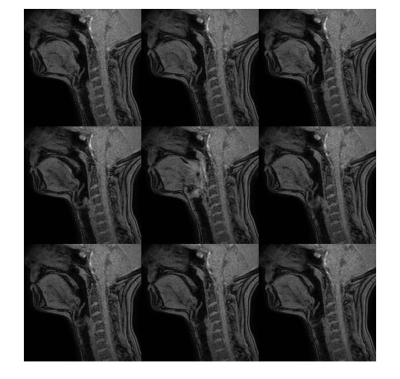
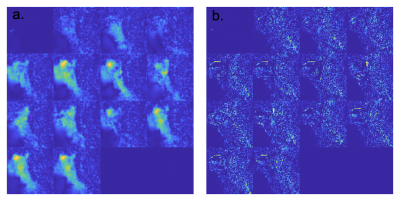
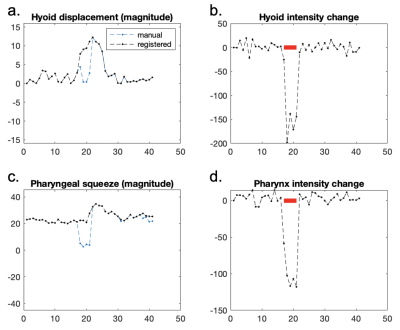
Ten adult subjects consisting of five gastrostomy-dependent patients who had undergone radiotherapy for head and neck cancer and five healthy volunteers were imaged on a 3T Philips Ingenia scanner. Subjects were directed to undertake a series of dry swallows while lying in the scanner, with the scan operator asking the patient to swallow immediately once the sequence had audibly commenced. Each swallow was imaged using a 2D gradient echo acquisition without spoiling (flip angle 5°, TR 2.51ms, TE 1.26ms, acquisition matrix 132x112, pixel size 0.83x0.83mm, slice thickness 10mm, averages 1) at a temporal resolution of seven frames per second. The acquisition plane was altered for each swallow such that three sagittal images (one midline and two paramedian), two axial images (at the level of the tongue base and cricoid cartilage) and one coronal image were acquired. We acquired standard T2-weighted and T1-weighted spin echo images for anatomical assessment.The sagittal midline images were temporally cropped to remove long time segments without swallows. The frame providing the closest match to the median image from the full time series was designed as the reference frame. All frames were registered to the reference image using joint registration and modelling of intensity changes, yielding deformation fields and intensity change maps, as previously described [3]. Regions-of-interest (ROIs) were placed on the reference frame using a dedicated graphical user interface (GUI) and propagated onto all frames using the registration deformation fields. ROIs were placed at the symphysis menti, hyoid bone, pre-epiglottic fat and crossing the oropharynx (Figure 1). Following registration, each frame was manually inspected to determine the accuracy of the registration for each ROI, and inaccurate ROIs were corrected. The performance of the registration was measured in terms of registration success, defined as the proportion of frames not needing manual adjustment for each of the ROIs.
We also investigated excluding frames with ‘extreme’ intensity changes due to unsaturated tissue being pulled into the slice during the largest movements of the swallow, because registration of these frames is difficult. For each ROI, any frame outside of the range of mean intensity ± three standard deviations from the first ten frames (before the swallow commenced) was designated as an extreme intensity frame. In the oropharynx, these frames can be considered to have length zero as the oropharynx is typically fully constricted when these intensity changes occur. For the combined registration and extreme intensity correction, registration success was defined as the proportion of frames that were either registered successfully (no manual correction needed) or could be excluded after being identified as having an extreme intensity change.
Results and Discussion
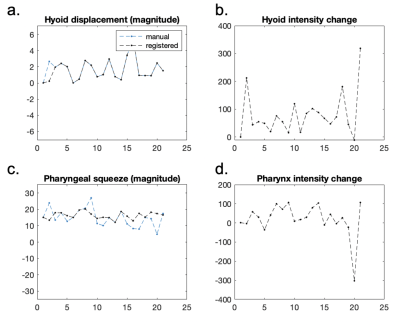
Examples of a series of images from a healthy volunteer are shown in Figure 2; the corresponding deformation field and intensity change maps are shown in Figure 3. Example displacement-time and intensity-time plots for a healthy volunteer and a patient with post-radiotherapy dysphagia are shown in Figures 4 and 5. Healthy volunteer swallows typically consisted of a single discrete swallowing motion, whereas swallows in post—radiotherapy patients often showed repeated but lower amplitude movements. Registration was accurate in the majority of frames but challenging during the swallow itself, where large tissue movements caused unsaturated tissue to be ‘pulled’ into the imaging slice, resulting in increased image intensity. The mean (SD) registration success was 77% (31%) at the hyoid, 77% (31%) at the pre-epiglottic fat and 44% (26%) at the tongue base. Success improved to 79%, 79% and 51% respectively after consideration of extreme intensity changes.Conclusions
Quantitative analysis of swallow function using registration and modelling of intensity changes is feasible in patients and volunteers and is accurate in the majority of frames. Registration can therefore reduce the time taken to analyse the images – which would otherwise require manual ROI placement on every frame – and could facilitate the analysis of swallow function. Capturing the very large movements during the height of the swallow is problematic due to large anatomical deformations and unsaturated tissue being pulled into the imaging slice. However, intensity analysis can identify frames with ‘extreme’ intensity changes where registration alone is unable to capture the swallowing motion and provides a complementary approach to assessment of swallow function.Acknowledgements
TJPB is supported by an National Institute for Health Research Clinical Lectureship. This work was undertaken at UCLH/UCL, which receives funding from the UK Department of Health’s the National Institute for Health Research (NIHR) Biomedical Research Centre (BRC) funding scheme. The views expressed in this publication are those of the authors and not necessarily those of the UK Department of Health.References
1. King SN, Dunlap NE, Tennant PA, Pitts T. Pathophysiology of Radiation-Induced Dysphagia in Head and Neck Cancer. Vol. 31, Dysphagia. 2016. p. 339–51.
2. Eisbruch A, Lyden T, Bradford CR, Dawson LA, Haxer MJ, Miller AE, et al. Objective assessment of swallowing dysfunction and aspiration after radiation concurrent with chemotherapy for head-and-neck cancer. Int J Radiat Oncol Biol Phys. 2002;53(1):23–8.
3. Odille F, Menys A, Ahmed A, Punwani S, Taylor SA, Atkinson D. Quantitative assessment of small bowel motility by nonrigid registration of dynamic MR images. Magn Reson Med. 2012;68(3):783–93.
Figures