3940
Application of Compressed Sensing Technology in the Fast Spin Echo Diffusion Weighted Imaging of the Skull Base1Department of Radiology, the First Affiliated Hospital of Dalian Medical University, Dalian, China, 2PHILIPS——Philips Healthcare, beijing, China
Synopsis
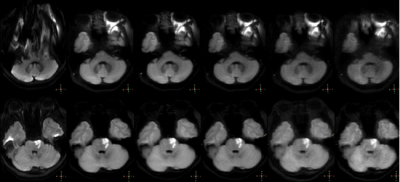
Compared with echo planar imaging diffusion weighted iamging (EPI-DWI), turbo spin echo diffusion weighted imaging (TSE-DWI) can significantly reduce magnetic sensitivity artifacts in skull base imaging. However, the longer scan time limits its clinical promotion. The purpose of this study is to investigate the effect of the compression sensing acceleration factor on the image quality of TSE-DWI in the skull base area.
Introduction
Diffusion weighted imaging (DWI), as one of the most commonly used MR functional sequences for the diagnosis of brain diseases, can non-invasively quantify the diffusion characteristics of water molecules using ADC1. The traditional DWI sequence uses echo planar imaging (EPI) technology, which can complete whole brain imaging in a short time. However, due to the variation of the magnetic field in the skull base area, it is prone to susceptibility artifacts and misdiagnosis2. DWI imaging based on turbo spin echo sequence (TSE) can eliminate magnetic sensitivity artifacts, but the scan time is relatively long, which limits its clinical promotion3. Compressed sensing (CS) can significantly shorten the scan time through sparse sampling, while ensuring the image quality to meet the diagnostic requirements4. The purpose of this study is to explore the effect of the compressed sensing acceleration factor on the image quality of the fast spin echo diffusion weighted imaging in the skull base area.Materials and methods
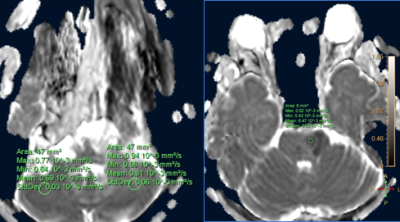
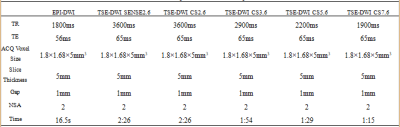
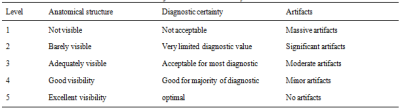
The study population consisted of 24 healthy subjects(8 females, 53.4±18 years), 22 subjects with dentures(8 females, 57.8±19.7 years) and 13 subjects with skull base lesions(8 females, 45.1±19.7 years), defined as group A, B, and C, Respectively. All subjects underwent the EPI-DWI and TSE-DWI scan of Skull Base on a 3.0 T MR scanner (Ingenia CX, Philips Healthcare, Best, the Netherlands). TSE-DWI adopted a routine clinical setup of SENSE acceleration factor 2.6, and CS factors of 2.6, 3.6, 5.6 and 7.6. Other scan parameters were shown in Table 1. Regions of interest were placed manually at both sides of the cerebellar hemisphere or unilateral lesion by two experienced radiologists for the measurement of ADC. The two observers used a five-point scoring method to evaluate the quality of the images (the scoring system was listed in Table 2). The Kappa test was adopted to evaluate the consistency of the scores from the two radiologists. If the consistency was in good agreement, the corresponding images would be adopted for further analysis by senior physicians. In the following analysis, the Kruskal-Wallis test was used to assess the difference of ADC and score between groups, and the Mann-Whitney U test was employed to make a pairwise comparison. This study has been approved by the local IRB.Results
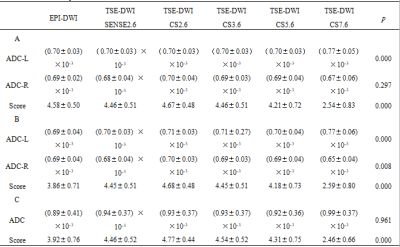
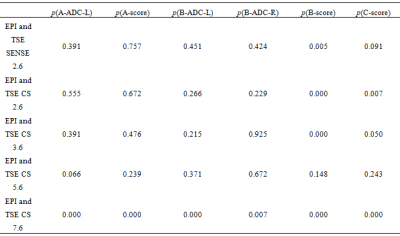
The scores by the two observers were in good agreement (p=0.509). In Table 3, it was shown that there were statistically significant differences in ADC-L and score of group A, ADC-L, ADC-R and score of group B, scores of group C. In Table 4, the ADC-L, score of group A and B were significantly different from the conventional sequences when CS factor was equal to 7.6, and scores of group B and C were significantly different from the corresponding conventional sequences when CS factor was equal to 2.6, 3.6. However, when CS=2.6, 3.6, the subjective score is higher than the conventional sequence.Discussion and Conclusions
Scan time for the skull base TSE-DWI could be reduced significantly by CS technique. However, if a large CS acceleration factor (≥7.6) is used, the image quality degrades evidently. CS acceleration factor of 5.6 is recommended for clinical skull base TSE-DWI to achieve an optimal balance between imaging time and image quality.Acknowledgements
No acknowledgement found.References
1. Kolff-Gart, AS; Pouwels, PJ; Noij, DP, et al. Diffusion-weighted imaging of the head and neck in healthy subjects: reproducibility of ADC values in different MRI systems and repeat sessions.AJNR Am J Neuroradiol,2015,36(2):384-390.
2. Wan Q, Lei Q, Wang P, et al. Intravoxel Incoherent Motion Diffusion-Weighted Imaging of Lung Cancer: Comparison Between Turbo Spin-Echo and Echo-Planar Imaging. J Comput Assist Tomogr,2020,44(3):334-340.
3. Elefante, A; Cavaliere, M; Russo, C, et al. Diffusion weighted MR imaging of primary and recurrent middle ear cholesteatoma: an assessment by readers with different expertise. Biomed Res Int,2015,2015:597896.
4. Bratke, G; Rau, R; Weiss, K, et al. Accelerated MRI of the Lumbar Spine Using Compressed Sensing: Quality and Efficiency. J Magn Reson Imaging,2019,49(7):e164-e175.
Figures