3938
The clinical value of magnetic resonance imaging in patients with sudden hearing loss for pathogenic diagnosis and prognostic evaluation1Radiology, Zhongda Hospital, School of Medicine, Southeast University, Nanjing, China, 2Philips Healthcare, Greater China, Shanghai, China
Synopsis
This study aimed to assess the clinical importance of 3D-FLAIR MR imaging in sudden sensorineural hearing loss (SSNHL) for head and neck radiologists and otolaryngologists. A novel MR protocol based on 3D-FLAIR and detailed clinical examinations were conducted among 60 patients. The results showed that the 3D-FLAIR MR protocol could identify the proper causes of SSNHL and reflect the severity of hearing loss, and the combination of clinical and MR features is beneficial for the prognostic evaluation of unilateral SSNHL, mainly for SSNHL with no recovery and complete recovery.
INTRODUCTION
Sudden sensorineural hearing loss (SSNHL) is one of the most common acute symptoms in the otolaryngology department. Pathogenic diagnosis is the premise of effective treatment of SSNHL, and prognostic evaluation is the key. However, about 85% patients are diagnosed as idiopathic due to a lack of overall assessment, and prognostic factors of SSNHL are numerous and remain controversial.1,2 Although 3D-FLAIR MR is increasingly applied for the diagnosis and prognosis of SSNHL, it is not widely used in clinical practice, mainly due to the following reasons: 1) clinicians and radiologists have not realized the value of MR enough, and there is a lack of standardized MR examination scheme; 2) the value of the combination of clinical features and MR findings for prognostic evaluation is rarely reported.3 The aim of the current study was to further validate the potential value of a MR protocol based on 3D-FLAIR in the pathogenic diagnosis of SSNHL, and to build a primary model based on clinical and MR features for the prognostic evaluation of unilateral SSNHL.METHODS
A prospective study was conducted in consecutive patients from May 2019 to August 2020. All patients were hospitalized, underwent detailed clinical evaluations and MR examinations, received proper pathogenic diagnosis. All MR examinations were performed on a 3.0T scanner (Philips Ingenia, Philips Healthcare, Best, The Netherlands) with the following protocol: T1WI-TSE, 3D-T2WI, DWI, post-contrast 3D-T1WI, pre-contrast and 4-hour delayed-enhanced 3D-FLAIR. Patients with unilateral SSNHL, except those with retrocochlear lesions, underwent the same comprehensive therapeutic regimen. Besides pathogenic diagnosis, the associations of MR findings with clinical features among patients with unilateral SSNHL were assessed by single factor analysis. The signal intensity ratio (SIR) of the affected ear was compared with that of the healthy one on delayed-enhanced 3D-FLAIR images. The SIR was defined as the signal intensity of the cochlea, vestibule, and auditory nerve divided by that of the ipsilateral cerebellum. For the prognostic evaluation of patients with unilateral SSNHL, two-labled classifications were adopted, including the recovery and no recovery groups, and the complete recovery and incomplete recovery groups. Significant clinical and MR features were compared and screened out by single factor analysis. The prognostic model was built by logistic regression analysis. A receiver operating characteristic curve was generated for efficiency assessment.RESULTS
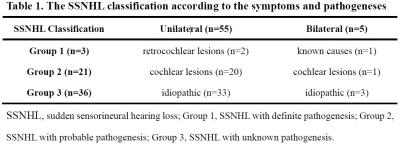
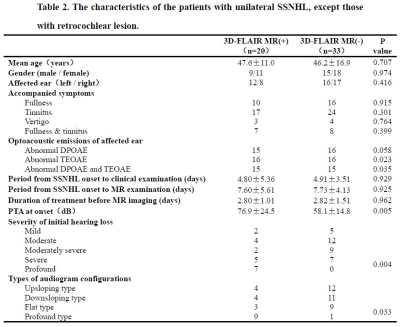
A total of 60 patients were enrolled and had proper pathogenic diagnoses. Among them, 53 patients with unilateral SSNHL, except those with retrocochlear lesions, were divided into the MR (+) and MR (-) groups (Table 1). Comparison of clinical characteristics between the two groups and the statistically significant features were shown in Table 2. The results of comparing multiple clinical and MR features between the recovery and no recovery groups and those between the complete recovery and incomplete recovery groups were shown in Table 3. Two primary clinical-image prognosis assessment models were built successfully, for the prediction of no hearing recovery and complete hearing recovery, respectively. The detailed prognostic factors and efficiency assessment of both models were shown in Figure 1. Figure 2 showed a case demonstrating the process of pathogenic diagnosis and prognosis assessment.DISCUSSION
We found that 24 patients (40%) had abnormal MR findings, which were related to SSNHL by the developed 3D-FLAIR MR protocol. This rate was higher than those reported in previous studies (11%–37.7%).4 It indicated that the novel MR protocol may be more useful for pathogenic diagnosis than 3D-FLAIR alone. By comparing clinical features between the MR (+) and MR (-) groups, the MR (+) group had higher incidence rates of severe to profound hearing loss, profound and flat type audiogram configurations and higher PTA values. Furthermore, quantitative analysis showed that the SIRs of the affected ear significantly differed between the MR (+) and MR (-) groups, as well as between the affected and healthy ears.These findings were positively correlated with the degree of initial hearing loss, suggested that extensive damage to inner ear structures correlates with a positive result on 3D-FLAIR, corroborating a previous study.4,5 For the prognostic evaluation of patients with unilateral SSNHL, some clinical and MR features have been reported to be related to prognosis, and high signal intensity on 3D-FLAIR was shown to be associated with poorer hearing especially.6 Accordingly, this study screened out significant clinical and MR features correlating with no recovery and complete recovery, respectively. During the process of building a prognosis assessment model for no hearing recovery in unilateral SSNHL, we found that adding the factor “positive MR inner ear findings” could improve the accuracy and efficiency of the model, further confirming that 3D-FLAIR MR was an indispensable prognostic tool. For the prognostic prediction of complete hearing recovery, the period from onset to MR examination was identified as a key factor, in line with the hypothesis of Conte G et al7 that 3D-FLAIR MR imaging abnormalities are more easily detected before steroid treatment initiation, indicating that MR imaging should be performed as soon as possible.CONCLUSION
The proposed 3D-FLAIR MR protocol is useful for pathogenic diagnosis and positive 3D-FLAIR findings with SIRs measurement can reflect the severity of initial hearing loss. The combination of clinical and MR features is beneficial for the prognostic evaluation of unilateral SSNHL.Acknowledgements
There is no special acknowledgement for this study.References
- Chandrasekhar SS, et al. Clinical Practice Guideline: Sudden Hearing Loss (Update). Otolaryngol Head Neck Surg 2019;161(1_suppl):S1-S45.
- Kuhn M, et al. Sudden sensorineural hearing loss: a review of diagnosis, treatment, and prognosis. Trends Amplif 2011;15(3):91-105.
- Conte G, et al. MR Imaging in Sudden Sensorineural Hearing Loss. Time to Talk. AJNR Am J Neuroradiol 2017;38(8):1475-1479.
- Min X, et al. Clinical value of abnormal MRI findings in patients with unilateral sudden sensorineural hearing loss. Diagn Interv Radiol 2020;26(5):429-436.
- Lee JI, et al. Prognostic Value of Labyrinthine 3D-FLAIR Abnormalities in Idiopathic Sudden Sensorineural Hearing Loss. AJNR Am J Neuroradiol 2016;37(12):2317-2322.
- Lammers MJW, et al. The prognostic value and pathophysiologic significance of three-dimensional fluid-attenuated inversion recovery (3D-FLAIR) magnetic resonance imaging in idiopathic sudden sensorineural hearing loss: A systematic review and meta-analysis. Clin Otolaryngol 2019; 44(6):1017-1025.
- Conte G, et al. MR Imaging in Sudden Sensorineural Hearing Loss. Time to Talk. AJNR Am J Neuroradiol 2017;38(8):1475-1479.
Figures

According to Siegel's criteria, the degree of recovery was classified as follows: complete recovery, final hearing threshold <25 dB; partial recovery, final hearing range of 25‐45 dB with >15 dB hearing gain; slight recovery, final hearing threshold >45 dB with >15 dB hearing gain, and no recovery, final hearing level >75 dB with <15 dB hearing gain.
Recovery group, including the patients with slight recovery, partial recovery and complete recovery.
Incomplete recovery group, including the patients with no recovery, slight recovery and partial recovery.
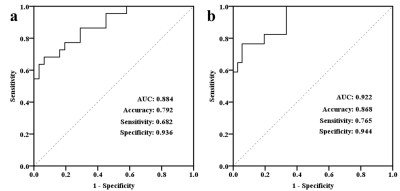
ROC curves of the two primary clinical-image prognosis assessment models for unilateral SSNHL.
Fig a. Model used for no hearing recovery with a moderate prediction value. It included six prognostic factors: age ≥ 50 years, simultaneously abnormal DPOAE and TEOAE, longer period from onset to clinical examination, PTA at onset, severe to profound initial hearing loss, and positive MR inner ear findings. Fig b. Model used for complete hearing recovery with a high prediction value. It consisted of two prognostic factors: PTA at onset and the period from onset to MR examination.
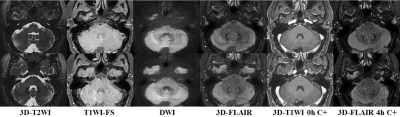
A 43ys patient presenting with SSNHL and tinnitus of the left ear for 7 days. The PTA was 80 dB. 3D-FLAIR images was scanned 3 days later, showed that SIs of the left cochlea and vestibule were slightly higher than those of the right with markedly delayed enhancement after contrast. Other sequences showed no abnormality. This case was diagnosed as unilateral SSNHL due to labyrinthine inflammation combined with blood labyrinth barrier disruption. The patient was hospitalized and received a comprehensive therapeutic protocol for 9 days, the curative effect was ineffective as expected.