3906
Head-to-head comparison of PSMA-PET/CT and ferumoxtran-10-enhanced MRI for the diagnosis of lymph node metastases in prostate cancer patients1Medical Imaging, Radboudumc, Nijmegen, Netherlands
Synopsis
In this head-to-head comparison study, 45 prostate cancer patients underwent both USPIO-enhanced MRI (nano-MRI) and prostate-specific membrane antigen PET/CT for the purpose of lymph node staging. The results of both scans were compared on number, size and location of suspicious lymph nodes. Both modalities identified suspicious LNs which were missed by the other. Both modalities identified suspicious LNs in all anatomical regions of the pelvis, however nano-MRI appeared to be superior in detecting smaller suspicious LNs.
Introduction
Assessing lymph node (LN) involvement in prostate cancer (PCa) patients is critical for prognosis and patient management. The current gold standard for LN-staging, pelvic lymph node dissection (PLND), is an invasive procedure and its curative and diagnostic performance are questioned. In the pursuit for less invasive and more accurate staging methods several imaging modalities including ferumoxtran-10 enhanced MRI (nano-MRI) and prostate-specific membrane antigen (PSMA)-PET/CT, have been evaluated for their performance and accuracy. Recently, the first large prospective study evaluating the accuracy of PSMA-PET/CT in patients with primary PCa reported a sensitivity and specificity of 85% and 98%, respectively for nodal and distant metastases (1). Nano-MRI relies on the accumulation of ultra-small super paramagnetic iron-oxide (USPIO) particles in healthy LNs, resulting in a hypointense signal on T2* - weighted imaging, whereas suspicious LNs (occupied by metastatic tissue) reflect a hyperintense signal. In the past nano-MRI demonstrated a comparable sensitivity (82%) and specificity (93%) (2). Since both modalities rely on different biology of LN metastases, the aim of this study was to evaluate their findings in terms of size, number and anatomical localisation of suspicious LNs in order to understand the diagnostic potential of these techniques in the detection of LN metastases in PCa patients.Methods
This study was approved by the local ethical review board and need for informed consent was waived. The medical files of patients with either primary PCa or recurrent disease who were referred for nano-MRI at our centre and also underwent a PSMA-PET/CT between October 2015 and July 2017, were retrospectively analysed. Both scans were performed at the same institution according to local protocols. PSMA-PET/CT imaging was carried out using 68Ga-PSMA-HBED-CC at 2 MBq/kg bodyweight, imaging after 60 minutes with whole body low-dose-CT for attenuation correction and anatomical referencing. Three-dimensional T2*-weighted nano-MRI was performed at isotropic resolution of 0.85x0.85x0.85 mm3 with a combined multi-gradient echo sequence with average TE of 12 ms, 24-36 hours after slow-drip intravenous infusion of ferumoxtran-10 (weight adapted dosage of 2.6 mg Fe/kg body weight) diluted in 100mL sodium chloride. All scans were analysed independently by experienced nuclear physicians/radiologists. Of all suspicious lesions, size, anatomical location and Level of Suspicion (LoS) on a likelihood scale ranging from 1 (no metastasis) to 5 (very high probability of metastasis) were determined. Subsequently, findings from PSMA-PET/CT and nano-MRI were compared.Results
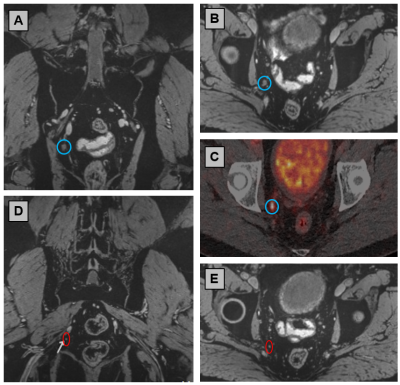
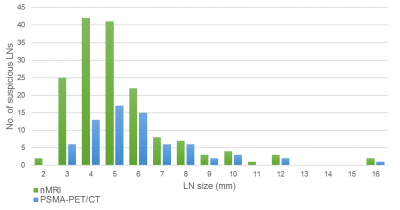
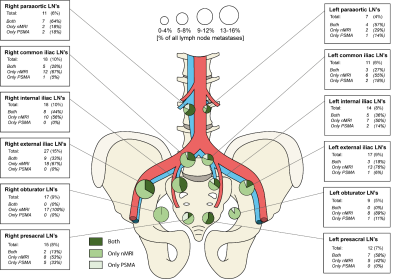
A total of 45 patients were included (example in Fig. 1); 8 primary PCa patients (mean PSA 28.9 ng/ml, ± 49.3) and 33 patients with recurrent PCa (mean PSA 5.0 ng/ml, ± 9.6). For one patient no historical data was available. Both scans were performed within a mean of 2 days (range 1-18 days) apart. A cumulative total of 179 suspicious LNs was identified, of which 160 were identified by nano-MRI in 33 patients, and 71 were identified by PSMA-PET/CT in 25 patients. Significantly more suspicious LNs were detected by nMRI (p<0.001). The mean size of the suspicious LNs as identified by nMRI was significantly smaller than those detected by PSMA-PET/CT (p=0.006). The distribution of suspicious LN size as identified by the individual modalities is depicted in figure 2. Mean LoS was similar for both modalities (p=0.493). The anatomical location did not show notable differences between both modalities (Fig. 3). 43% of all identified suspicious LNs were located outside the standard PLND-template. Of all LNs, 108 were only identified by nMRI (60%), 52 (29%) were detected by both methods, and 19 (11%) were identified only by PSMA-PET/CT.Discussion
By comparing the results of two imaging modalities in the same patient population, this study aimed to evaluate the potential of a combined diagnostic role for PSMA-PET/CT and nano-MRI. The findings of this head-to-head comparison, imply a benefit from a complementary use, most pronounced in small LNs. As sensitivity of PSMA-PET/CT in essence depends on PSMA-expression, this could explain of the failing of the detection of lesions with a too low PSMA-expression level. On the other hand, nano-MRI relies on lymphotropic affinity of ferumoxtran-10 by cells of the immune system, which accumulate the contrast agent in healthy LNs. Thus, in case of disturbance of accumulation in non-metastatic tissue, e.g. by fibrosis, the discriminative ability between metastatic and non-metastatic tissue in nano-MRI could be impaired. Ideally, a reference standard should be used to evaluate those results and such research is strongly encouraged, but this surpasses the scope of the current study. Nevertheless, the results of this study underline the importance of understanding both the technical capabilities of imaging techniques in combination with tumour biology in order to interpret the imaging results appropriately.Conclusion
The present study evaluated and compared the findings of PSMA-PET/CT and nano-MRI and demonstrated that the differences between their findings were mostly related to the average size of the identified LNs. Although a prospective study with a standard of reference is warranted for confirmation, the results of this study provide important insight in a potential complementary role of both imaging modalities and may be considered in clinical diagnostic decisions.Acknowledgements
No acknowledgement found.References
1. Hofman MS, Lawrentschuk N, Francis RJ, et al. Prostate-specific membrane antigen PET-CT in patients with high-risk prostate cancer before curative-intent surgery or radiotherapy (proPSMA): a prospective, randomised, multicentre study. Lancet. 2020;395:1208-1216.
2. Heesakkers RA, Hovels AM, Jager GJ, et al. MRI with a lymph-node-specific contrast agent as an alternative to CT scan and lymph-node dissection in patients with prostate cancer: a prospective multicohort study. Lancet Oncol. 2008;9:850-856.
Figures