3875
The feasibility of reduced field-of-view DWI in evaluating bladder invasion of uterine cervical cancer
Mayumi Takeuchi1, Kenji Matsuzaki2, and Masafumi Harada1
1Department of Radiology, Tokushima University, Tokushima, Japan, 2Department of Radiological Technology, Tokushima Bunri University, Sanuki, Japan
1Department of Radiology, Tokushima University, Tokushima, Japan, 2Department of Radiological Technology, Tokushima Bunri University, Sanuki, Japan
Synopsis
Uterine cervical cancer with urinary bladder invasion is classified as stage IVA with poor prognosis. Cystoscopy is a diagnostic procedure but relatively invasive examination. MRI can rule out the bladder invasion and skipping cystoscopy may be possible, however, high false positive rate may be problematic. The bladder mucosal invasion in 14 cases was evaluated with reduced FOV DWI (rFOV-DWI) and compared with cystoscopic findings. The diagnosis of invasion had a sensitivity of 100%, specificity of 50%, accuracy of 93%, PPV of 92%, and NPV of 100%. Addition of rFOV-DWI may improve the staging accuracy in assessing the bladder mucosal invasion.
Introduction
Uterine cervical cancer with urinary bladder mucosal invasion classified as FIGO stage IVA represent about 2% of cases. Cystoscopy is a diagnostic procedure in evaluating the bladder mucosal invasion of cervical cancer, however, it is relatively invasive examination with risk of complications. MRI has a high diagnostic accuracy for ruling out the presence of bladder mucosal invasion, with NPV of 100% 1, 2. The absence of bladder mucosal invasion can be diagnosed with sufficient confidence and skipping cystoscopy based on MRI is safe enough without concern for under-staging. On the other hand, the high rate of false positive cases on MRI (PPV of 7-38%) to avoid under-staging may be problematic 1, 2. DWI demonstrates cervical cancer as a high signal intensity mass, however, detailed evaluation of bladder invasion on conventional DWI is occasionally difficult due to low spatial resolution, and distortion. Reduced phase direction field-of-view (FOV) technique by using spatially selective phase encoding gradient can offer high quality DWI with improved spatial resolution, without associated phase wrap round artifact, and with less artifacts related to motion and susceptibility which are common in conventional DWI 3-6. The purpose of this study is to evaluate the diagnostic performance of reduced FOV DWI (rFOV-DWI) in evaluating bladder mucosal invasion of cervical cancer compared with cystoscopic findings.Methods
14 women (mean age, 66 years) with histologically proven cervical cancer (12 squamous cell carcinomas and 2 adenocarcinomas) who were undergone both cystoscopy and MRI including T2WI, and rFOV-DWI (FOCUS: FOV optimized and constrained undistorted single shot, FOV:20-24*10-12cm, Matrix:160*80, thickness:5mm, b = 50 and 800 sec/mm2) with 3T MRI units (Discovery MR750, GE Healthcare) were included in the study (Table 1). The border between the tumor and the bladder wall was visually evaluated on T2WI and rFOV-DWI as “clear” or “unclear”, and the presence of bladder mucosal invasion was visually evaluated on both sagittal, and oblique axial or oblique coronal rFOV-DWI and corresponding ADC map with the consensus of two readers. The results were compared with the cystoscopic findings.Results and Discussions
The 14 cervical cancers included FIGO stage IIIB (2 cases), IVA (5 cases), and IVB (7 cases) tumors. Mean maximum tumor diameter measured on MRI was 79 mm (range 50-150 mm). In all 14 cases, the border between the tumor and the bladder wall was unclear on T2WI and clear on rFOV-DWI (Fig. 2). 13 of 14 cases were positive for bladder mucosal invasion on rFOV-DWI, and cystoscopic finding revealed the bladder mucosal invasion in 12 of the 13 cases with positive mucosal invasion on rFOV-DWI (Fig. 3). Whereas the other two cases (one positive and one negative cases on rFOV-DWI) were negative mucosal invasion on cystoscopy (Fig. 4, 5). The diagnosis of bladder mucosal invasion based on rFOV-DWI findings had a sensitivity of 100%, specificity of 50%, accuracy of 93%, PPV of 92%, and NPV of 100%.According to the guidelines for the staging of uterine cervical cancer with MRI, T2WI is essential, however, tumors sometimes are not well delineated on T2WI and the use of contrast medium or DWI may be recommended. In our study, T2WI showed insufficient contrast between the bladder wall and the tumor, making it difficult to assess the extent of invasion. Park et al. reported high diagnostic ability in assessing the parametrial invasion of cervical cancer on fused T2WI and DWI 7. Takeuchi et al. reported that rFOV-DWI could define the tumor margins and demonstrate local extension of cervical cancer more accurate than T2WI 6. In our study, the bladder mucosal invasion was clearly demonstrated on rFOV-DWI with high PPV (92%) and it is considered that rFOV-DWI may improve the staging accuracy of cervical cancer.
Contrast-enhanced MRI may also be useful in the evaluation of local tumor extension of cervical cancer, however, gadolinium-containing contrast agents may not be available due to renal dysfunction, which is often present due to hydronephrosis. Therefore, rFOV-DWI, which allows assessment of bladder invasion without the use of contrast agents, may be highly useful.
Conclusion
Addition of rFOV-DWI may improve the staging accuracy of MRI for cervical cancer in assessing the bladder mucosal invasion.Acknowledgements
No acknowledgement found.References
- Rockall AG, et al. Can MRI rule out bladder and rectal invasion in cervical cancer to help select patients for limited EUA? Gynecol Oncol. 2006;101:244-249.
- Kim WY, et al. Reliability of magnetic resonance imaging for bladder or rectum invasion in cervical cancer. J Reprod Med. 2011;56:485-490.
- Bhosale P, et al. Feasibility of a reduced field-of-view diffusion-weighted (rFOV) sequence in assessment of myometrial invasion in patients with clinical FIGO stage I endometrial cancer. J Magn Reson Imaging 2016;43:316-324.
- Takeuchi M, et al. Evaluating Myometrial Invasion in Endometrial Cancer: Comparison of Reduced Field-of-view Diffusion-weighted Imaging and Dynamic Contrast-enhanced MR Imaging. Magn Reson Med Sci. 2018;17:28-34.
- Ota T, Hori M, Onishi H,et al. Preoperative staging of endometrial cancer using reduced field-of-view diffusion-weighted imaging: a preliminary study. Eur Radiol. 2017;27:5225-5235.
- Takeuchi M, et al. Reduced field-of-view diffusion-weighted MR imaging for assessing the local extent of uterine cervical cancer. Acta Radiol. 2020;61:267-275.
- Park JJ, et al. Parametrial invasion in cervical cancer: fused T2-weighted imaging and high-b-value diffusion-weighted imaging with background body signal suppression at 3 T. Radiology 2015;274:734-741.
Figures
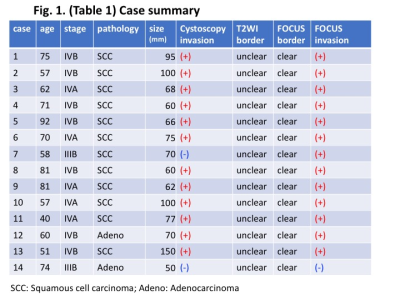
Table 1: Case summary
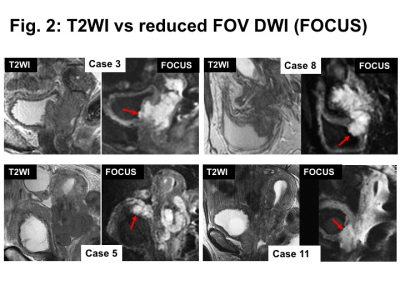
T2WI vs reduced FOV DWI (FOCUS): The border between the tumor and the bladder wall was unclear on T2WI and clear on rFOV-DWI.
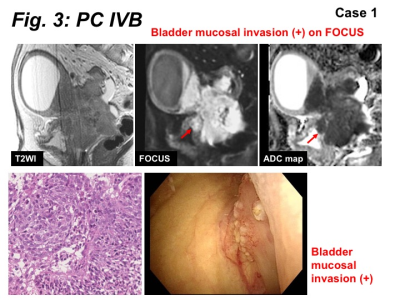
Bladder mucosal invasion positive case: Bladder mucosal invasion was positive on rFOV-DWI, and confirmed by cystoscopy.
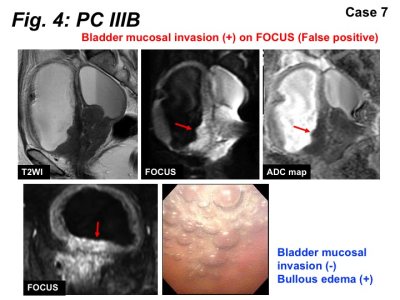
Bladder mucosal invasion false positive case: Bladder mucosal invasion was positive on rFOV-DWI, but not confirmed by cystoscopy (false positive). Probably submucosal invasion with bullous edema may mimic mucosal invasion on rFOV-DWI.
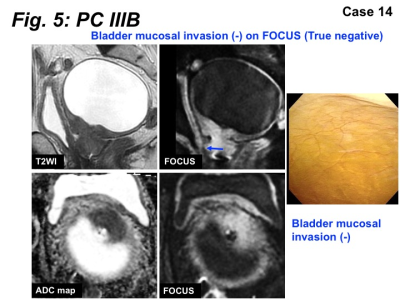
Bladder mucosal invasion negative case: Bladder mucosal invasion was negative on rFOV-DWI, and confirmed by cystoscopy.