3863
Spectral-Heterogeneity-Adaptive Radiofrequency Pulses for Improving the Conspicuity of Meniscal Tears at 3T and 7T1Siemens Medical Solutions USA, Inc., Rochester, MN, United States, 2Department of Radiology, Mayo Clinic, Rochester, MN, United States
Synopsis
In this work, we evaluate the efficacy of Spectral-Heterogeneity-Adaptive Radiofrequency Pulses (SHARP)-based partial fat saturation for improving meniscal pathology conspicuity at 3T and 7T. Under the guidelines of an IRB, 11 subjects with knee meniscal pathology detected on a previous 3T MRI were imaged at 3T and 7T using six different turbo spin-echo–based MRI imaging options that included SHARP. Two fellowship-trained musculoskeletal radiologists evaluated meniscal pathology conspicuity and selected the top three preferred options for each case. SHARP improved conspicuity of meniscal pathology at 3T and 7T and was within top three preferred options for the highest number of times.
Introduction
Suppression of fat signal is extensively used in clinical musculoskeletal MRI to improve the conspicuity of pathology (1–3). Spectral fat saturation has better time efficiency compared to Dixon methods which are more robust to non-uniformity of the main magnetic field (B0). B0 variation, however, results in non-uniform spectral fat saturation. Spectral-Heterogeneity-Adaptive Radiofrequency Pulses (SHARP)(4)-based partial fat saturation was recently proposed to improve uniformity of spectral fat saturation, and was used with Subtle Intensity Graduating Homomorphic Transform (SIGHT) to improve meniscal pathology conspicuity at 7T (5).The purpose of this work is to evaluate the efficacy of SHARP-based partial fat saturation for improving meniscal pathology conspicuity at both 3T and 7T. In a previous study, preliminary evaluation of SHARP’s efficacy for improving conspicuity of meniscal pathology was presented for 5 subjects imaged at 3T and 7T using 3 different imaging options (6). This work extends the evaluation to 11 subjects imaged at both 3T and 7T using six different imaging options.
Methods
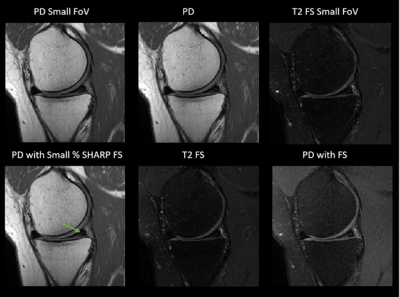
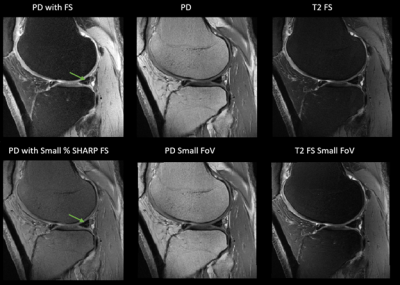
ImagingUnder the guidelines of an IRB, 11 subjects who had knee meniscal pathology detected on a previous 3T MRI were imaged at 3T and 7T using six different turbo spin-echo–based MRI imaging options that included SHARP. The six different imaging options were: i) Proton density–weighted MRI (PD); ii) PD with small field-of-view (PD Small FoV); iii) T2-weighted MRI with chemical shift selective (CHESS) fat saturation (T2 FS); iv) T2 FS with small field-of-view (T2 FS Small FoV; v) PD with CHESS FS (PD with FS); vi) PD with small percentage SHARP fat saturation (PD with SHARP FS).
Imaging was performed at 3T on a MAGNETOM Skyra (Siemens Healthcare, Erlangen, Germany) using a single-channel transmit, 15-channel phased-array receive knee coil (Quality Electrodynamics, Mayfield Village, OH, USA), and at 7T on a MAGNETOM Terra (Siemens Healthcare, Erlangen, Germany) using a single-channel transmit, 28-channel phased-array receive knee coil (Quality Electrodynamics, Mayfield Village, OH, USA).
A prototype 2D turbo spin-echo sequence was developed for applying fat saturation using SHARP with functionality to change fat-saturating radiofrequency pulse’s center frequency offset (compared to water), bandwidth, and flip angle. SHARP was used to apply a small percentage of fat saturation as described earlier (6).
Evaluation
Two fellowship-trained musculoskeletal radiologists (co-authors with experience of 16 and 10 years) evaluated meniscal pathology conspicuity in a blinded and randomized study and selected the top three preferred options among the six options for each case. The images with larger field-of-view were zoomed to the same size as the smaller field-of-view images for blinded evaluation.
Results
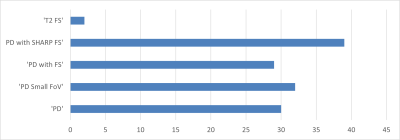
Figure 1 shows the comparison of the different imaging options evaluated in this study in a representative subject scanned at 3T. Improved conspicuity of meniscal pathology can be observed with SHARP fat saturation. Figure 2 shows a similar comparison in another subject imaged at 7T.Figure 3 shows the clustered bar chart for the different options evaluated by the radiologists for meniscal pathology conspicuity. PD with small-percentage SHARP fat saturation was selected 39 times within the top three options out of a total of 132 opportunities (2 radiologists x 2 field strengths x 11 subjects x 3 preferences). SHARP was one of the top three preferred options 29.5% of the times, 12.9% more times than each option being equally likely (16.6%). T2 FS (chosen two times) and T2 FS with small field-of-view (never chosen) were the least preferred options for detecting meniscal pathology. PD, the option currently used clinically at our institution, was chosen 22.7% times. PD with small field-of-view and PD with the typical (CHESS) fat saturation were selected 24.2% and 22% percent of times, respectively. Based on the cumulative counts, PD with small-percentage SHARP fat saturation, PD with small field-of-view, and PD were the top three preferred options in order.
Discussion
The effects of hyper-intense fat (in bone marrow near the menisci) coupled with receive coil sensitivity–induced hypo-intensity at the center of the field-of-view could reduce the conspicuity of intra-meniscal signal, which is used as one primary criterion for detecting meniscal pathology. The modulation of the intensity of fat by using SHARP and applying a small percentage of fat saturation improved the dynamic range of intensities around the menisci, thus improving the conspicuity of meniscal pathology.Fat near the surface of the knee is more hyper-intense than fat at the center of the field-of-view due to surface coil flare. PD with small field-of-view avoids the hyper-intense fat near the surface and improves the dynamic range of intensities for better detection of meniscal pathology. But with SHARP, more anatomy is available for clinical evaluation. PD with typical (CHESS) fat saturation also improves the dynamic range of intensities for better conspicuity of the meniscal pathology, but significantly alters the contrast of the PD images that are typically used without fat saturation for identifying meniscal pathology. Additionally, PD with CHESS fat saturation has higher specific absorption rate (SAR) than SHARP with small percentage fat saturation. SHARP improved the dynamic range without reducing the field-of-view or altering the contrast and SAR significantly.
Conclusions
SHARP-based partial fat saturation has potential to improve meniscal pathology conspicuity without altering the field-of-view or significantly increasing SAR.Acknowledgements
No acknowledgement found.References
1. Delfaut EM, Beltran J, Johnson G, Rousseau J, Marchandise X, Cotten A: Fat suppression in MR imaging: Techniques and pitfalls. Radiographics 1999.
2. Sage JE, Gavin P: Musculoskeletal MRI. Vet Clin North Am - Small Anim Pract 2016; 46:421–451.
3. Del Grande F, Santini F, Herzka DA, et al.: Fat-Suppression Techniques for 3-T MR Imaging of the Musculoskeletal System. RadioGraphics 2014; 34:217–233.
4. Chebrolu VV, Frick M, Kollasch P, et al.: Fat Saturation in Musculoskeletal MRI using Spectral Heterogeneity Adaptive RF Pulses (SHARP). In Proc Jt Annu Meet ISMRM-ESMRMB; 2018:5174.
5. Chebrolu VV, Kollasch P, Stinson EG, et al.: Subtle Intensity Graduating Homomorphic Transform with a Small-percentage of Fat-saturation to Improve Conspicuity of Meniscal Tears at 7T. In ISMRM SMRT Virtual Conf; 2020:2801.
6. Chebrolu VV, Kollasch P, Howe B, et al.: Improving the Conspicuity of Meniscal Tears in Knee MRI at 3T and 7T. In Proc 27th Sci Meet Int Soc Magn Reson Med. Montréal, QC, Canada; 2019:1397.
Figures