3828
Accelerating Neuroradiology Protocols with Deep Learning MR Image Reconstruction. Which Methods Result in the Highest Perceived Image Quality?1University of Wisconsin School of Medicine and Public Health, Madison, WI, United States, 2GE Healthcare, Madison, WI, United States
Synopsis
Deep Learning (DL) MRI image reconstruction holds great promise in improving overall MRI image quality and decreasing examination time. Given the nonlinear properties of DL reconstruction it is unknown which methods of decreasing MRI examination time are most suitable when adapting current protocols for DL based examination acceleration. 10 volunteers were scanned with clinical baseline T1 and T2 weighted FSE exams, along with 5 accelerated exam types. The resulting exams were scored to determine differences in image quality. DL image reconstruction allowed for an up to 78% reduction in scan time while matching baseline subjective image quality.
Introduction
Deep Learning (DL) MRI image reconstruction holds great promise in creating images with improved spatial resolution, decreased ringing artifact, and significantly improved SNR.1 Applying a DL reconstruction to a conventionally acquired examination results in an examination with improved image quality. However, current protocols are by design intended to have sufficient SNR and resolution for most common imaging indications. An equal (or greater) clinical need is to image patients in less time resulting in less motion, improved workflow efficiency, and improved patient satisfaction. Given the nonlinear properties of DL reconstruction it is unknown which common methods of decreasing examination time (decreasing NEX, decreasing matrix size, increasing parallel imaging acceleration factor, or a combination) are most applicable when adapting current protocols for DL based examination acceleration. This work tests multiple acceleration strategies to determine which result in the highest perceived image quality for neuroimaging when compared to clinical standard T1 and T2 FSE based techniques.Methods
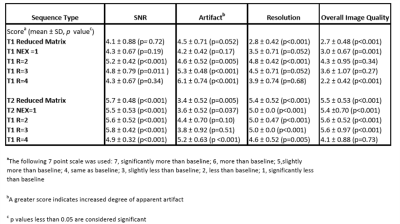
A total of 10 volunteers were imaged for this Institutional review board (IRB) approved study and all volunteers gave written informed consent for participation.MRI Acquisition and Image Reconstruction: All MRI images were obtained on a single 3.0 Tesla system (Discovery MR 750, GE Healthcare, Waukesha, WI) utilizing a 32 channel head coil (Nova Medical Systems, MA, USA). Baseline T1 and T2 FSE sequences were generated by minor modifications from current clinical protocols. The baseline MRI parameters are provided in Figure 1. These baseline parameters were then modified by the following interventions: reducing NEX to 1, reducing matrix size (T1:320 x 150, T2: 256 x 170), and increasing overall parallel imaging acceleration factors (R) to 2, 3 and 4 times the baseline exam. This resulted in 10 separate accelerated acquisitions, split five with T1 and five with T2 weighting. For each volunteer the two baseline sequences were acquired first, followed by alternating T1 and T2 weighted accelerated sequences. Each image set was processed with both conventional Fourier transform based reconstruction and a prototype version deep learning based reconstruction designed to reduce noise and improve resolution.2
Image Analysis: Three neuroradiologists (15, 13, and 8 years of radiology experience, respectively) independently analyzed the resulting images. The observers were blinded to the acceleration technique utilized for each image and subjectively compared each evaluation image set to the reference Fourier transform reconstructed image set. Images were evaluated for perceived resolution, artifact, SNR, and overall image quality on a 7 point Likert scale, with a “4” on the Likert scale being judged to be the same as the refence image set.
Statistical Analysis: The median values of the three radiologists’ scores were analyzed. Differences in scores as compared to the expected baseline score were tested using a one sample t-test. Pairwise differences in scores among the acceleration techniques were assessed using a t-test for dependent samples. P values <0.05 were considered statistically significant for comparison to the expected baseline score, while a Bonferroni-corrected p value of < 0.0056 was considered significant for the multiple pairwise comparisons.
Results
The denoising properties of the DL recon were uniformly effective, with all protocols having non-inferior or superior subjective SNR compared to the baseline exam. Three of the accelerated protocols were statistically non-inferior with regards to subjective SNR and 7 out of the 10 demonstrated statistically superior subjective SNR compared to the baseline examinations.Subjective resolution was also considered similar or better than the baseline exam in 9 out of the 10 protocols, with only the reduced matrix T1 weighted images judged to have lower subjective resolution than the baseline images.Parallel imaging artifacts impaired the performance of the accelerated T1 weighted images, with three out of the five T1 weighted images having statically significant increase in these artifacts. Conversely, only the most accelerated T2 weighted image (acceleration factor 4) demonstrated a statically significant increase in artifact.
Overall T2 weighed image quality was non-inferior or superior to the baseline study with all accelerated techniques. The T2 weighted image with acceleration factor of 4 was non-inferior to the baseline and all other protocol acceleration changes were statically superior compared to the baseline exam. Overall T1 image quality was decreased compared to the baseline exam when performed with an acceleration factor of 4, a NEX of 1, or reduced matrix size. Accelerated T1 weighted overall image quality was unchanged compared to baseline with parallel imaging acceleration factors of 2 and 3.
Conclusion:
Deep learning image reconstruction is a valuable method to improve the speed and image quality of head MRI. This technique facilitated a substantial reduction in imaging time while maintaining overall image quality. In general, reduction in NEX and judicious parallel imaging acceleration resulted in greater overall image quality compared to reduction in matrix size and more aggressive parallel imaging acceleration techniques. T2 weighted DL accelerated sequences were more uniformly successful in generating images with high perceived image quality as compared to the T1 weighted images, which could be in part due to the higher native SNR of the baseline sequence. Further investigation is warranted to optimize protocol parameters for use with deep learning reconstruction to achieve the best clinical combination of speed and image quality.Acknowledgements
No acknowledgement found.References
1. Lundervold AS, Lundervold A. An overview of deep learning in medical imaging focusing on MRI. Z Med Phys. 2019 May;29(2):102-127.
2. Lebel RM. Performance characterization of a novel deep learning-based MR image reconstruction pipeline. 2020 Aug 14 [accessed 2020 Dec 15]. https://arxiv.org/abs/2008.06559v1
Figures
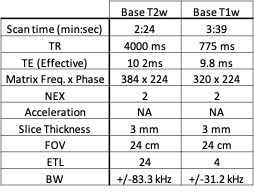
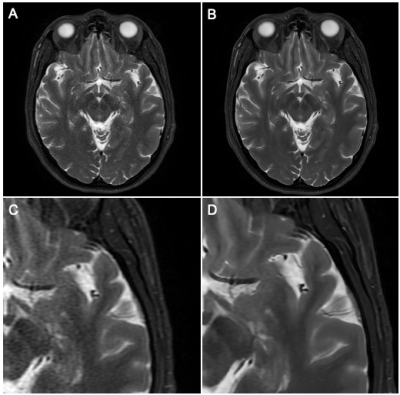
Figure 1. Demonstration of Deep Learning Reconstruction Technique
A. Parallel imaging acceleration factor of 4, conventional Fourier transform reconstruction, 78% reduction in acquisition time from the baseline sequence with increased noise.
B. Same acquisition as in figure A, deep learning reconstruction demonstrating reduction of apparent noise to less than baseline exam with DL reconstruction technique
C. Magnified detail view of A.
D. Magnified detail view of B.
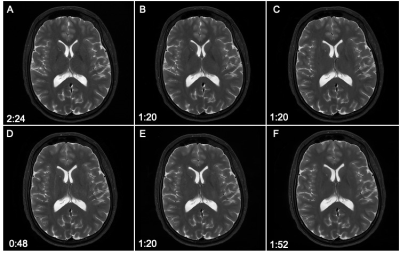
Figure 2. T2 Weighted Comparisons
A. Baseline T2w FSE – time to acquire 2:24
B. R=2 T2w FSE – time to acquire 1:20
C. R=3 T2w FSE – time to acquire 1:20
D. R=4 T2w FSE – time to acquire 0:48
E. NEX=1 T2w FSE – time to acquire 1:20
F: Reduced Matrix T2w FSE – time to acquire 1:52