3813
Evaluating the role of T2-weighted-imaging in acute ischemic stroke to accelerate routine Stroke-MRI protocol1Clearmedi Healthcare Pvt. Ltd., Gurugram, India, 2Department of Radiology, Paras Hospitals, Gurugram, India, 3Philips Health Systems, Philips India Limited, Gurugram, India
Synopsis
The focus of MRI stroke-research is concentrated in identifying relevant sequence for stroke-screening, accelerating the acquisitions by latest innovations like Compressed-SENSE and developing methodologies to extract meaningful clinical-relevance (i.e., penumbra or mismatch-ratio) using minimum number sequences. Our objective is to evaluate the impact of including T2-weighted-images in fast acute-ischemic-stroke MRI protocols, to comment on role of T2w vis-à-vis Flair in terms of clinical findings for making an informed decision on the inclusion-criteria of ideal MR sequences in stroke MR protocol. Flair proves to be better than T2, in depicting small/subtle signal changes in critical time-window, beneficial for acute-stroke patient-treatment-planning.
AIMS and objective
Optimization of fast comprehensive MR imaging protocol for evaluating the acute ischemic stroke has been studied extensively in the past few years [1-2] . The focus area of MRI stroke research has been concentrated in identifying relevant sequence for stroke screening, accelerating the acquisitions by means of latest innovations like Compressed-SENSE and developing methodologies to extract meaningful clinical relevance (i.e, penumbra or mismatch-ratio) using minimum number sequences [3]. The first crucial step in stroke-screening, however, happens to be optimizing which sequence to include and at what time-compensation cost. While, several stroke-centres use T2-weighted-imaging as part of the standard stroke-MRI protocol; on the other hand, it has been observed that a number of centres are adopting 5-minutes stroke protocols by omitting T2w scans [4]. This choice of inclusion still remains to be a decision made by the radiologist, and not derived from any systematically observed clinical study [5]. Our objective is to evaluate the impact of including T2-weighted images in fast acute-ischemic-stroke MRI protocols, to comment on the role of T2w vis-à-vis Flair in terms of clinical findings for making an informed decision on the inclusion criteria of ideal MR sequences in stroke MR protocol.Materials and methods
In this retrospective study, approved by local ethics committee, acute-ischemic-stroke MRI protocol included DWI, Flair, SWI, T2w, and non-contrast MR angiography imaging. The sequence details are summarized in Table-1. Twenty-two acute stroke patients were scanned by this protocol, on a 3.0 T wide-bore MRI (Ingenia, Philips Health Systems, Best, The Netherlands) using a 15 channel head coil. Two radiologists with more than 15+ years of experience in neuro-imaging, blinded to the clinical information, evaluated the findings on both sequences (Flair and T2w). Contribution of T2w and Flair findings in the final diagnosis was compared in terms of percentage in three segments: i) Stroke-onset-time within 3-8 hours of the critical window, ii) Stroke-onset-time < 3-8 hours, iii) Stroke-onset-time > 3-8 hours. Clinical findings are represented in Table-1.Results
i) In 36% cases (8 out of 22), where the Stroke-onset-time was within 3-8 hours of critical window, the Flair images were ranked to be superior in terms of lesion hyper-intensity and signal-change detection in image quality. In these cases, Flair images were able to delineate the subtle or severe hyper-intense lesions, whereas T2w images had shown no signal-changes or very subtle changes respectively. ii) For 18% of cases (4 out of 22), the findings were matching negatively, i.e., both Flair and T2w demonstrated no reported signal change. These 18% cases suggested and later confirmed, of the Stroke-onset-time being < 3-8 hours. iii) In remaining 45% of cases (10 out of 22), Stroke-onset-time > 3-8 hours; findings on Flair and T2 were exactly matching in detecting hyper-intensity of lesion as well as in terms of image quality.Discussion
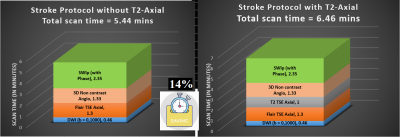
T2w images are usually included in stroke protocol to detect ischemic infarction appearing as hyperintense lesion usually seen within the first 3–8 hours after stroke onset. This mismatch between positive DWI and negative Flair/T2w can be useful in identifying the patients who might particularly benefit from timely thrombolysis therapy. Our findings specifically highlight the superiority of Flair imaging over T2w, in demonstrating small/ subtle intensity changes if present, in this 3-8 hours window. This happens to be a very critical time-point from patient-management perspective. Thus the superiority of Flair justifies that T2w can actually be removed from the protocol to tailor it as per time-constraints of this window-period. For identifying lesions in stroke onset time < 3-8 hours, both Flair and T2w performances were similar in finding no hyper-intense lesion. Also for cases, where both Flair and T2w report similar hyper-intensity of lesions, are in the onset time > 3-8 hours window. Therefore, Flair shows promising results in terms of patient criticality in all the three possible scenarios and is likely to be better than T2w. Flair can reliably ensure that T2w can be omitted from existing acute-stroke MRI protocol without affecting critical findings at any of these time-windows. This can, in turn, save an additional 14% of scan time (1 minute out of 7 minutes), which is quite important in acute stroke patient management.Conclusion
Flair proves to be better than T2, in depicting small/subtle signal changes in critical time-window, beneficial for acute-stroke patient treatment planning. This helps in favour of the strong informed decision of omitting T2w from non-invasive stroke-MRI protocols, thus saving 14% scan time and making the protocol faster for patient benefit, even more at par with CT scan time.Acknowledgements
No acknowledgement found.References
[1] K. Nael et al., “Six-minute magnetic resonance imaging protocol for evaluation of acute ischemic stroke: Pushing the boundaries,” Stroke, vol. 45, no. 7, pp. 1985–1991, 2014.
[2] R. Jagsi et al., “HHS Public Access,” vol. 263, no. 2, pp. 219–227, 2017.
[3] J. P. Villablanca et al., “Magnetic Resonance Imaging Detection of Microbleeds Before Thrombolysis,” Stroke, vol. 33, no. 1, pp. 95–98, 2002.
[4] X. Zhang et al., “A fast multiparameter MRI approach for acute stroke assessment on a 3T clinical scanner: preliminary results in a non-human primate model with transient ischemic occlusion.,” Quant. Imaging Med. Surg., vol. 4, no. 2, pp. 112–11222, 2014.
[5] C. Leiva-Salinas and M. Wintermark, “Imaging of Ischemic Stroke Carlos,” Neuroimaging Clin N Am, vol. 20, no. 4, pp. 455–468, 2010.