3734
Longitudinal Registration of Knee MRI Based on Femoral and Tibial Alignment1Electrical Engineering, Zhejiang University, Hangzhou, China, 2Bioengineering, University of Washington, Seattle, WA, United States, 3Radiology, University of Washington, Seattle, WA, United States
Synopsis
This study aims to develop an automatic and robust algorithm for longitudinal registration of knee Magnetic Resonance Imaging (MRI) across the time span of eight years. We propose a technique that firstly achieves rigid registration based on femoral segmentation, and then makes evaluations based on tibial alignment. Both qualitative and quantitative results show solid performance of the proposed algorithm. This registration algorithm lays a solid foundation for serial analysis of knee images taken over a multi-year time frame.
Introduction
Longitudinal registration of MRI data is fundamental to follow disease progression and regression overtime. In the context of vessel wall and atherosclerotic plaque imaging, with proper registration, researchers and clinicians can measure and compare changes of key morphological and compositional parameters of plaques at the same anatomical location.The publicly available OsteoArthritis Initiative (OAI) [1] dataset, which contains 4796 subjects with up to 7 annual time points MRI, offers unique opportunity to study vascular pathobiology [2]. However, before summarizing the progression/regression pattern of vessel walls and plaques across such a long-term time course, an automatic and robust algorithm for multi-timepoint registration of popliteal artery is required.
Existing methods [3-4] register arteries directly, but these non-rigid approaches stretch and distort the blood vessels while doing alignment, which is undesirable for longitudinal analysis. Instead, we need a method that rigidly registers the knee structure which is assumed to change the least among different anatomies. Then the location of popliteal artery, especially in the longitudinal direction, is naturally aligned.
Inspired by the observation that the essence of longitudinal registration of knee MRI is to register femur, tibia and their relative positions, we develop a novel knee joint registration algorithm based on femoral and tibial alignment.
Methods
14 subjects (including images from 83 time points in total) from OAI are analyzed in the study.The registration workflow consists of two parts: (a) longitudinal registration based on femoral mask, and (b) quantitative evaluation based on tibial mask.
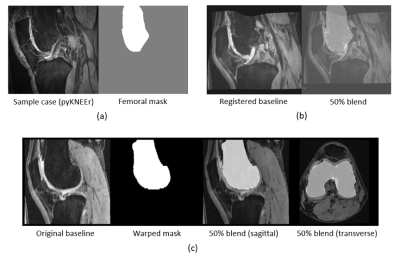
Femur-based registration: Firstly, all knee MR images are standardized to RAI (right, anterior, inferior) orientation and left laterality. Then, each baseline knee joint is automatically segmented to generate a femoral mask. The segmentation is based on non-rigid registration, where each knee is first mapped to a sample case, and the manually pre-segmented femoral mask of this sample case is then warped by the inverse transform. An illustration of the femur segmentation is shown in Fig 1. The codebase and sample case from the pyKNEEr study [5] is used. Finally, based on the assumption that there are only rigid displacements within the femur of same patients across eight years, the knee at the following time points is rigidly registered to the baseline femur.
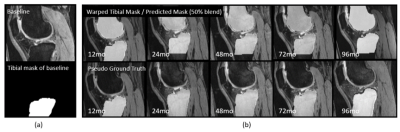
Tibia-based evaluation: Firstly, we manually annotate the tibial mask of the pyKNEEr sample case. Secondly, registration-based segmentation, as introduced above, is applied to all time points in order to obtain the ‘pseudo’ ground truth of tibial masks. We call them ‘pseudo’ because they are generated, but they can function just like the ground truth annotated. Thirdly, the femur-based rigid transformation is used to warp each baseline tibial mask to all following time points. Finally, the warped tibial masks are compared to the ‘pseudo’ ground truth using average Hausdorff distance (indicating how well two contour edges match), dice score (indicating how well two masks overlap) and maximum longitudinal offset (difference between the largest coordinates in the longitudinal direction of the two masks). The registration result with dice score lower than 0.8 or with average Hausdorff distance larger than 0.2 mm (maximum Hausdorff distance in the absence of distal tibia) is marked as failure.
Previously, an analysis technique for popliteal artery vessel wall evaluation (FRAPPE) [6] was developed which can generate centerline coordinates of popliteal arteries in standardized knee MR images. Warping FRAPPE centerlines with the corresponding rigid transform, the centerline deviation at different time points is calculated and thus vessel alignment can be evaluated.
Results
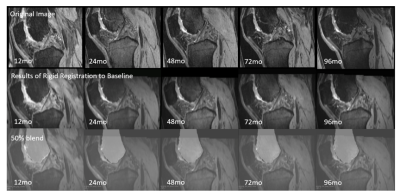
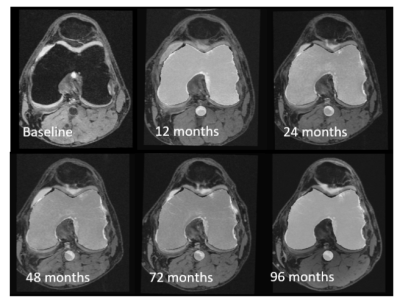
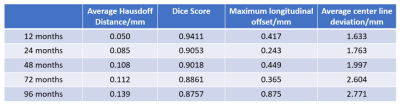
An example of femur-based knee registration is shown in Fig 2 and Fig 3, in sagittal and transverse view respectively.The results of tibia-based quantitative evaluation of registration are shown in Table 1. An example of warped tibial masks from baseline to later time points is also shown in Fig 4.
There are four cases (5.8%) that are detected as failure, all from time point of 96 months, which are excluded in Table 1. The registration algorithms show low average Hausdorff distances (<0.14mm), high dice scores (>0.87) and low maximum longitudinal offsets (<0.5mm except 96 months), which indicates that the two masks match well.
The vessel centerline deviation is also presented in Table 1 and illustrates good performance of our knee registration algorithm.
Discussion and Conclusion
In this work, we proposed a femur-based registration method for knee MRI and showed that knees scanned at multiple annual timepoints can be registered well. Through tibia-based evaluation, the algorithm is capable of automatically detecting failed cases which may require manual adjustments otherwise.Interestingly, with longer time span, the performance of registration has a certain degree of decline because of the year-by-year changes of the knee joint including femur, tibia, cartilage, soft tissue, etc. which posts a challenge. However, even at the time point of 96 months, the maximum longitudinal offset of tibia is less than 1mm, which is satisfactory.
This algorithm has laid the groundwork for future analysis of atherosclerotic plaque development. Even though it is developed for knees, it may be applied to other anatomical regions where bone structures can be used to assess the global motion between scans.
Acknowledgements
No acknowledgement found.References
[1] Fawaz-Estrup F. The osteoarthritis initiative: an overview. Med Health R I. 2004;87:169–171.
[2] Liu, Wenjin, et al. "Understanding Atherosclerosis Through an Osteoarthritis Data Set: From Knee to Vessel." Arteriosclerosis, thrombosis, and vascular biology 39.6 (2019): 1018-1025.
[3] Biasiolli, Luca, J. Alison Noble, and Matthew D. Robson. "Multicontrast MRI registration of carotid arteries in atherosclerotic and normal subjects." Medical Imaging 2010: Image Processing. Vol. 7623. International Society for Optics and Photonics, 2010.
[4] Wu, Yu-Xia, et al. "Multi-contrast MRI registration of carotid arteries based on cross-sectional images and lumen boundaries." Medical Imaging 2017: Image Processing. Vol. 10133. International Society for Optics and Photonics, 2017.
[5] Bonaretti, Serena, Garry E. Gold, and Gary S. Beaupre. "pyKNEEr: An image analysis workflow for open and reproducible research on femoral knee cartilage." Plos one15.1 (2020): e0226501.
[6] Chen, Li, et al. "Fully automated and robust analysis technique for popliteal artery vessel wall evaluation (FRAPPE) using neural network models from standardized knee MRI." Magnetic Resonance in Medicine (2020).
Figures