3692
The relationship between pubic and levator ani muscle injury among primiparas after vaginal delivery:A pelvic floor MRI study1Tianjin first central hospital, tianjin, China, 2Tianjin first central hospital, Tianjin, China
Synopsis
To explore the relationship between pubic injury and levator anal muscle(LAM) injury among primiparas after vaginal delivery. 88 primiparas after vaginal delivery were collected in our study. Two radiologists identified and evaluated the injury condition of pubic and LAM on MR images. The proportion of LAM injury was significantly higher in the pubic injury group than that of in the non-pubic injury group, and the degree of pubic injury was positively correlated with the degree of LAM injury.
Purpose
Vaginal delivery may cause injury of multiple structures that constitute the birth canal, such as bony birth canal: pubic separation, fracture; soft birth canal: levator ani muscle(LAM) injury, and etc[1-2]. Pubic injury has significant clinical symptoms,such as tenderness and barriers to action, while LAM injury are covert and without obvious clinical symptoms, but LAM injury is the most important reason for pelvic floor dysfunction disease, so our study was aimed to explore the relationship between pubic and LAM injury and make sure if the bony canal injury can suggests the soft birth canal injury even though without significant clinical symptoms.Methods
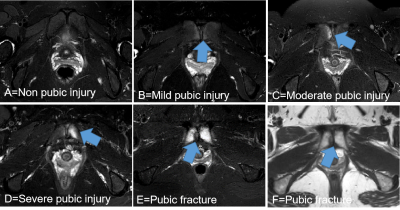
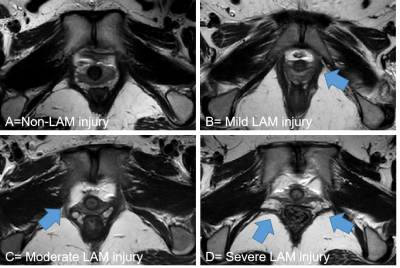
88 primiparas after vaginal delivery at postpartum 42 days were prospective collected and underwent static MRI(Ingenia, Philips Healthcare, the Netherlands). Two radiologists identified and evaluated the injury condition of pubic and LAM, including pubic bone marrow edema, pubic fractures, LAM tears, and scored their severity on pelvic floor images according to the criterion[3](Fig.1-2). The pelvic floor MR sequence included coronary and transverse mDIXON-T2WI: TR 4110 ms,TE 102 ms,FOV 260 mm×260 mm,matrix 320×256,thickness 3 mm,slice gap 0.3mm,NEX 2. The primiparas were separated to pubic injury group and non-pubic injury group according to pubic condition on MR images. Chi-square test was used to explore the difference in the proportion of LAM between two groups. Kendall`s tau-b correlation analysis was performed to explore the correlation between the score of pubic injury and the score of LAM injury.Result
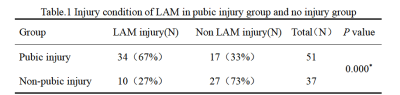
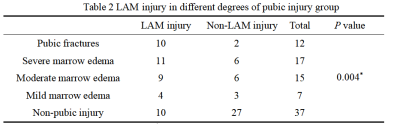
There was a significant difference in the incidence of LAM injury between the pubic injury group and the non-pubic injury group (67% vs 27%, P=0.000)(Table.1). The incidence of LAM injury varied according to the score of pubic bone injury (P=0.004)(Table.2). The primiparas with pubic fractures had higher rates of LAM injury. There was a positive correlation between the degree of pubic injury and the degree of LAM injury (P=0.036)(Fig.2).Discussion
The incidence of the pubic and LAM injury caused by vaginal delivery had correlation, the frontal portion of LAM attach to the both side of parapubic-symphysis area, pubic injury often occur near the pubic symphysis, which could easily cause LAM injury at the same time, the more serious the pubic injury, the heavier LAM involvement will be.Conclusion
The pubic injury caused by childbirth is often associated with the LAM injury, and the degree of those injury are positively correlated. Obstetricians and gynecologists should pay attention to evaluate the LAM injury even though without obvious clinical symptoms when the primipara is clearly diagnosed with pubic injury.Acknowledgements
No acknowledgement found.References
[1]Turner Catherine E,Young Jane M,Solomon Michael J,Ludlow Joanne,Benness Christopher. Incidence and etiology of pelvic floor dysfunction and mode of delivery: an overview.[J]. Pubmed,2009,52(6).
[2]Agten Christoph A,Metzler Christoph,Rosskopf Andrea B,Zanetti Marco,Binkert Christoph A,Prentl Elke,Pfirrmann Christian W A. MR imaging of pubic symphysis after uncomplicated vaginal delivery and planned caesarean delivery in the first postpartum week.[J]. Pubmed,2019,56.
[3]Miller Janis M,Low Lisa Kane,Zielinski Ruth,Smith Abigail R,DeLancey John O L,Brandon Catherine. Evaluating maternal recovery from labor and delivery: bone and levator ani injuries.[J]. Pubmed,2015,213(2).